Abstract
Purpose
The aim of this study was to evaluate the frequency of various otolaryngological symptoms in patients with COVID-19 with regard to age, gender and pneumonia-related thorax CT characteristics.
Methods
This is a retrospective study conducted between March 25, 2020 and April 25, 2020. The anamnesis and medical files of 155 patients who applied to our outpatient COVID-19 clinic were evaluated. Patients with positive PCR tests for COVID-19 who were aged between 18–72 years were divided into groups according to the presence of otolaryngological symptoms. The differences between the two groups were examined.
Results
Of the 155 patients, 89 (57.4%) had otolaryngological symptoms. The mean age of the patients was 36.3 ± 8.1 years. Ninety-one (58.7%) patients were female, and 64 (42.2%) were male. Fifty-eight (37.4%) patients had received a clinical diagnosis of viral pneumonia with ground glass findings in tomography. The frequency of otolaryngological symptoms was higher in females than males (p: 0.029). The otolaryngological symptoms were also observed to be more frequent in the 18–30 age group (p: 0.013) compared to other age groups.
Conclusions
Tinnitus, gingivitis, sudden hearing loss, Bell’s palsy, and hoarseness can be seen in COVID-19, albeit rarely. Revealing the otolaryngological symptoms of COVID-19, and obtaining more information about the extent of disease will be useful in managing patients and their complaints associated with otolaryngology
Similar content being viewed by others
Introduction
The disease caused by the virus named as SARS-CoV-2 started in Wuhan, China at the end of 2019. It spread throughout the globe at an alarming pace and became the first pandemic of the twenty-first century. After seeing some signs of slowing with worldwide measures, it is evident that the disease (COVID-19) will continue to spread due to the reduction in strict measures [1].
It is well-established that the disease may be asymptomatic or may range from mild to very severe symptoms [2,3,4]. According to the data obtained in recent studies, the severity of the disease differs epidemiologically according to race, gender and age [2, 5, 6].
COVID-19 was classified as type A has seen in the USA and Australia, type B has seen in China, and East Asia and type C has seen in Europe in a recent study [7]. These subtypes can have different clinical symptoms as well.
In this study, we aimed to investigate otolaryngological symptoms in patients diagnosed with COVID-19 at our clinic.
Methods
We conducted a retrospective observational study in our hospital which was designated as a ‘pandemic hospital’ by the Ministry of Health, between March 25, 2020 and April 25, 2020. The study group was comprised of patients who had applied to our outpatient clinic and were later confirmed to have COVID-19 via real-time PCR (qRT-PCR) tests on respiratory samples (oropharyngeal and nasopharyngeal swabs). All patients between the ages of 18–72 were included in the study. The patient groups with otolaryngological symptoms were divided into 5 age groups: ages between 18–30 was defined as Group 1, ages between 30–40 was Group2, ages between 50–60 was Group 4 and ages more than 60 was defined as Group 5. The distribution of age according to ENT symptoms was evaluated. The extraction of RNA from samples was performed using the NucleoSpin® RNA Virus kit (Macherey–Nagel) according to the manufacturer’s instructions, and amplification via RT-PCR was performed with protocols developed by the Turkish National Public Health Institute [8].
We aimed to determine the frequency of various otolaryngologic symptoms in patients with COVID-19, and to evaluate these symptoms with regard to age, gender and thorax CT results.
Every patient who applied to our outpatient clinic first went through nurse triage. Body temperature (Medisana Thermometer 48,611), pulse and saturation (WristOx2 3150 Nonin Medical pulse oximeter) values of each patient who applied to our outpatient clinic were routinely measured and recorded by nurses before being subject to clinical examination by a physician. The oxygen saturations of the patients were also compared in this study. Then, the patients were given a two-page form to fill their medical history and complaints. (The language used in the form was easily understandable.) Any patients who had difficulty in filling the form were guided by nurses and physicians who provided explanatory support without leading or rushing the patients. In this form, the patients were first asked about the presence of additional diseases, allergies, use of alcohol or smoking, medications and any previous surgical history. In the next section of the form, detailed complaints were given in an easy to understand language with subheadings, including symptoms of the head and neck region, cardiovascular system, respiratory system, gastrointestinal system, genitourinary system, central nervous system and musculoskeletal system, and dermatological findings. The patients were asked to simply mark the complaints that they were experiencing at the time. The head and neck region complaints included the following: loss of odor and/or taste, sore throat, cough, nasal congestion, postnasal discharge, otalgia, tinnitus, hearing loss, oro-dental problems, vertigo, hoarseness and any other additional complaints. The patients were asked to simply mark all complaints that they were currently experiencing.
Detailed anamnesis, age, gender, follow-up studies, possible consultations with the infectious diseases and chest diseases departments, blood analysis results, tomography and PCR results were obtained from the electronic database of the hospital and Ministry of Health. All obtained results were examined in the current study.
This retrospective, archival, and the clinical study was conducted in line with the dictates of the World Medical Association Declaration of Helsinki with the informed consent of the participants and was approved by the local ethical committee.
Microsoft Excel and SPSS (Statistical Package for Social Sciences) Release 22.0 were used to evaluate the data. For all parameters, p ≤ 0.05 was considered statistically significant. Statistics for all data were presented as mean ± standard deviation, number and percentages. Fisher’s exact and Chi square tests were used in comparisons of categorical data.
Results
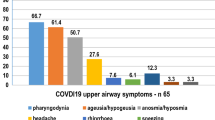
There were otolaryngological symptoms in 89 (57.4%) of 155 patients. Of these 89 patients, 55(35.4%) had anosmia, 25 (16.1%) had ageusia, 42 (27%) had sore throat, 68 (43.8%) had cough, 20 (12.9%) had nasal congestion, 10 (6%) had postnasal discharge, 4 (2%) had otalgia, 15 (9%) had runny nose, 2 (1.2%) tinnitus, 8 (5.1%) hoarseness, 2 (1.2%) had gingivitis, 1 (0.6%) had Bell’s palsy, 1 (0.6%) had sudden hearing loss problems (Table 1).
Ninety-one (58.7%) of the 155 patients were female, and 64 (42.2%) were male. Otolaryngologic (ENT) symptoms were seen at a higher frequency in females compared to males (p: 0.029) (Table 2).
Overall, 64 of the patients were hospitalized, while 91 were quarantined at home. Hospitalization criteria routinely included the presence of ground glass appearance in CT and conclusive findings of pneumonia. Other factors that were considered in the decision for hospitalization were: severe vomiting, resistant diarrhea, dyspnea, and progressive/resistant fever according to recent Ministry of Health guidelines.
When the comorbidities of the patients were examined, 28 hypertension (18%), 21 asthma (13.5%), 14 cardiovascular diseases (9.6%), chronic obstructive pulmonary disease 8 (5.1%), and other comorbid diseases were observed less frequently.
The average age of the group was 36.3 ± 8.1 years. When patient groups with otolaryngological symptoms were divided into 5 age groups, it was revealed that the ENT symptoms were mostly observed in the 18–30 years age group (p: 0.013) (Table 3).
Fifty-eight (37.4%) patients received a clinical diagnosis of pneumonia and had ground glass in tomography. There was no statistical difference in the frequency of pneumonia among COVID-19 patients with or without ENT symptoms (Table 4).
The patients’ oxygen saturation was 95.8% (± 3.2). There was no statistical significance in the saturations of patients with or without ENT symptoms (p: 0.85).
Discussion
COVID-19 disease is a new pandemic that occurs towards the end of 2019. Information about this disease was shared by China first, and then more information about the disease was obtained with its spread throughout Europe, especially Italy. However, since this pandemic is new, information about this disease is also limited.
Knowing the symptoms and percentages of the disease will help to discover COVID-19 disease more, and create more effective treatment protocols. There are recent general symptom studies on this topic. However, to our knowledge, detailed research on ENT symptoms is still more limited. Studies on COVID-19 revealed that ENT symptoms were observed more frequently in younger age groups, and women [9,10,11].
In general, studies on COVID symptoms indicate fatigue, cough, headache, fever, myalgia, arthralgia, and diarrhea [4, 12]. In our study, the symptoms of ENT were examined in more detail, and the highest percentage of ENT was cough (43.8%), and sore throat, and anosmia (35.4%). Unlike our study, Yonghyun et al. found anosmia in 15.3% of their patient group [13]. Based on our study, we can say the most significant predictive otolaryngologic symptoms are cough, anosmia, and sore throat.
In addition to the literature, the least common ENT symptoms were tinnitus in two patients, hoarseness in eight, and gingivitis in two patients. It is not known whether they are symptomatic of the disease or seen as an incidentally additive to the disease.
Of the 155 patients admitted to our outpatient hospital, 58 (37.4%) of them had ground glass appearance with pneumonia, and according to our government ministry of health care agency’s hospitalization algorithm, these patients were hospitalized. In other studies, this rate was found at 29.2% [12]. Two of our patients were taken to the intensive care unit. These patients did not show any ENT symptoms.
The retrospective nature of our study may not reflect the actual population since it does not include inpatients, and is of only one origin. The lack of knowledge of how the symptoms persist, the results of the treatment they receive create the limitations of our research. However, as far as it is known, the studies performed as isolated ENT symptoms on COVID-19 are limited. This study is the known first study in the literature that provides information on ENT symptoms, and age, gender, and pneumonia critters.
Currently, many hospitals in many countries around the world are working as pandemic quarantine hospitals, but as the number of COVID patients decreases, the measures taken are further relaxed, and the numbers of quarantine hospitals are decreasing for the current situation.
In this process, in which patient examination is increased with other diseases other than COVID-19 disease, it is recommended that ENT doctors and family physicians have an idea, and be more careful about these various symptoms of patients.
References
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ et al (2020) The origin, transmission, and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res 7(1):11
Singhal T (2020) A review of Coronavirus Disease-2019 (COVID-19). Indian J Pediatr 87(4):281–286
Wu Z, McGoogan JM (2020) Characteristics of, and important lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control, and prevention. JAMA 25(3):278–280
Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P et al (2020) Clinical, and epidemiological characteristics of 1,420 European patients with mild-to-moderate Coronavirus Disease. J Intern Med 1(2):120–157
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395(10223):497–506
Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, Liu S, Yang JK (2020) Gender differences in patients With COVID-19: focus on severity, and mortality. Front Public Health 8:152
Forster P, Forster L, Renfrew C, Forster M (2020) Phylogenetic network analysis of SARS-CoV-2 genomes. ProcNatlAcadSci USA 117(17):9241–9243
Tagliabue M, Pietrobon G, Ugolini S, Chu F, Ansarin M (2020) Nasopharyngeal swabs during SARS-CoV-2 pandemic: a role for the otolaryngologist. Eur Arch Otorhinolaryngol 1:7–8
Kai Chua AJ, Yun Chan EC, Loh J, Charn TC (2020) Acute olfactory loss is specific for COVID-19 at the emergency department. Ann Emerg Med 5:14
Vaira LA, Salzano G, Deiana G, De Riu G (2020) Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope 130(7):1787
Suzuki M, Saito K (2007) Min WP Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope 117(2):272–277
Gilani S, Roditi R, Naraghi M (2020) COVID-19, and anosmia in Tehran Iran. Med Hypotheses 141:109757
Yonghyun L, Pokkee M, Seonggu L, Shin W (2020) Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci 35(18):e174
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Health Ministry of Turkey Ankara, May2020 (IRB number: 2020-05-30T15_04_44).
Availability of data and material
Windows Excel + Pacs viewer software. From YıldırımBeyazit University Akgun viewer system.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elibol, E. Otolaryngological symptoms in COVID-19. Eur Arch Otorhinolaryngol 278, 1233–1236 (2021). https://doi.org/10.1007/s00405-020-06319-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06319-7