Abstract
Introduction
Salvage total laryngectomy (STL) is the most common treatment for recurrent laryngeal cancer after (chemo)-radiotherapy [(C)RT]. In this scenario, a higher rate of local wound complications, such as pharyngo-cutaneous fistula (PCF) and pharyngo-esophageal stenosis (PES), is generally expected. The aim of the present study is to evaluate outcomes using a standardized reconstructive protocol.
Methods
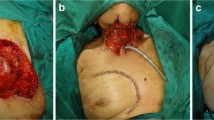
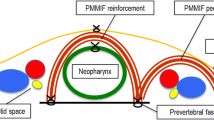
Between 2009 and 2019, patients undergoing STL after (C)RT were collected at two referral hospitals with the objective of evaluating surgical outcomes using a standardized reconstructive policy based on the use of fascio-cutaneous free flaps as inlay patch grafts and a long-lasting salivary bypass stent.
Results
Fifty-five patients (mean age, 66 years; male-to-female ratio, 8:1) were included in the study. Previous treatments were RT in 22 (40%) patients, CRT in 21 (38.2%), and partial laryngeal surgery followed by adjuvant (C)RT in 12 (21.8%). Reconstruction was accomplished by radial forearm and anterolateral thigh free flaps in 16 (29.1%) and 39 (70.9%) patients, respectively. Flap success rate was 98.2%. Concerning postoperative complications, we encountered 3 PCFs (5.4%) and 1 PES (1.8%).
Conclusion
The standardized reconstructive protocol analyzed herein granted significantly lower rates of PCF and PES after STL compared with data available in the literature.






Similar content being viewed by others
References
Forastiere AA, Goepfert H, Maor M et al (2003) Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 349:2091–2098
Steiner W, Vogt P, Ambrosch P, Kron M (2004) Transoral carbon dioxide laser microsurgery for recurrent glottic carcinoma after radiotherapy. Head Neck 26:477–484
Piazza C, Peretti G, Cattaneo A, Garrubba F, De Zinis LO, Nicolai P (2007) Salvage surgery after radiotherapy for laryngeal cancer: from endoscopic resections to open-neck partial and total laryngectomies. Arch Otolaryngol Head Neck Surg 133:1037–1043
Pellini R, Pichi B, Ruscito P et al (2008) Supracricoid partial laryngectomies after radiation failure: a multi-institutional series. Head Neck 30:372–379
Motamed M, Laccourreye O, Bradley PJ (2006) Salvage conservation laryngeal surgery after irradiation failure for early laryngeal cancer. Laryngoscope 116:451–455
Meulemans J, Delaere P, Nuyts S, Clement PM, Hermans R, Vander Poorten V (2017) Salvage transoral laser microsurgery for radiorecurrent laryngeal cancer: indications, limits, and outcomes. Curr Otorhinolaryngol Rep 5:83–91
Puxeddu R, Piazza C, Mensi MC, Ledda GP, Argiolas F, Peretti G (2004) Carbon dioxide laser salvage surgery after radiotherapy failure in T1 and T2 glottic carcinoma. Otolaryngol Head Neck Surg 130:84–88
Tsou YA, Hua CH, Lin MH, Tseng HC, Tsai MH, Shaha A (2010) Comparison of pharyngocutaneous fistula between patients followed by primary laryngopharyngectomy and salvage laryngopharyngectomy for advanced hypopharyngeal cancer. Head Neck 32:1494–1500
Hasan Z, Dwivedi RC, Gunaratne DA, Virk SA, Palme CE, Riffat F (2017) Systematic review and meta-analysis of the complications of salvage total laryngectomy. Eur J Surg Oncol 43:42–51
Microvascular Committee of the American Academy of O-H, Neck S (2019) Salvage laryngectomy and laryngopharyngectomy: multicenter review of outcomes associated with a reconstructive approach. Head Neck 41:16–29
Piazza C, Bon FD, Paderno A et al (2017) Fasciocutaneous free flaps for reconstruction of hypopharyngeal defects. Laryngoscope 127:2731–2737
Piazza C, Taglietti V, Nicolai P (2012) Reconstructive options after total laryngectomy with subtotal or circumferential hypopharyngectomy and cervical esophagectomy. Curr Opin Otolaryngol Head Neck Surg 20:77–88
Amin MB, Edge, S, Greene F, Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, Sullivan DC, Jessup JM, Brierley JD, Gaspar LE, Schilsky RL, Balch CM (2017) AJCC cancer staging manual. Springer International Publishing: American Joint Commission on Cancer
Redaelli de Zinis LO, Ferrari L, Tomenzoli D, Premoli G, Parrinello G, Nicolai P (1999) Postlaryngectomy pharyngocutaneous fistula: incidence, predisposing factors, and therapy. Head Neck 21:131–138
Basheeth N, O’’eary G, Sheahan P (2014) Pharyngocutaneous fistula after salvage laryngectomy: impact of interval between radiotherapy and surgery, and performance of bilateral neck dissection. Head Neck 36:580–584
Cecatto SB, Soares MM, Henriques T, Monteiro E, Moura CI (2014) Predictive factors for the postlaryngectomy pharyngocutaneous fistula development: systematic review. Braz J Otorhinolaryngol 80:167–177
Mattioli F, Bettini M, Molteni G et al (2015) Analysis of risk factors for pharyngocutaneous fistula after total laryngectomy with particular focus on nutritional status. Acta Otorhinolaryngol Ital 35:243–248
Suslu N, Senirli RT, Gunaydin RO, Ozer S, Karakaya J, Hosal AS (2015) Pharyngocutaneous fistula after salvage laryngectomy. Acta Otolaryngol 135:615–621
Dedivitis RA, Aires FT, Cernea CR, Brandao LG (2015) Pharyngocutaneous fistula after total laryngectomy: systematic review of risk factors. Head Neck 37:1691–1697
Liang JW, Li ZD, Li SC, Fang FQ, Zhao YJ, Li YG (2015) Pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis of risk factors. Auris Nasus Larynx 42:353–359
Sassler AM, Esclamado RM, Wolf GT (1995) Surgery after organ preservation therapy. Analysis of wound complications. Arch Otolaryngol Head Neck Surg 121:162–165
Weber RS, Berkey BA, Forastiere A et al (2003) Outcome of salvage total laryngectomy following organ preservation therapy: the radiation therapy oncology group trial 91-11. Arch Otolaryngol Head Neck Surg 129:44–49
Ganly I, Patel S, Matsuo J et al (2005) Postoperative complications of salvage total laryngectomy. Cancer 103:2073–2081
Sayles M, Grant DG (2014) Preventing pharyngo-cutaneous fistula in total laryngectomy: a systematic review and meta-analysis. Laryngoscope 124:1150–1163
Paleri V, Drinnan M, van den Brekel MW et al (2014) Vascularized tissue to reduce fistula following salvage total laryngectomy: a systematic review. Laryngoscope 124:1848–1853
Alexander FW (1963) Micropathology of Radiation Reaction in the Larynx. Ann Otol Rhinol Laryngol 72:831–841
Marx RE (1983) Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg 41:283–288
Sastre N, Rodriguez A, Blas R (1987) Skin flap neovascularization by means of a vasodilator. J Reconstr Microsurg 3:265–268
Ben-Yosef R, Kapp DS (1992) Persistent and/or late complications of combined radiation therapy and hyperthermia. Int J Hyperthermia 8:733–745
Aitasalo K, Aro HT, Virolainen P, Virolainen E (1992) Healing of microvascular free skin flaps in irradiated recipient tissue beds. Am J Surg 164:662–666
Kostakoglu N, Manek S, Terenghi G, Polak JM, Green CJ (1994) Free sensate secondary skin flaps: an experimental study on patterns of reinnervation and neovascularisation. Br J Plast Surg 47:1–9
Kostakoglu N, Terenghi G, Manek S, Batchelor AG, Polak JM, Green CJ (1995) Reinnervation and neovascularisation in prefabricated free muscle flaps. Microsurgery 16:388–395
Mathes SJ, Alexander J (1996) Radiation injury. Surg Oncol Clin N Am 5:809–824
Gibbs IC, Le QT, Shah RD, Terris DJ, Fee WE, Goffinet DR (2003) Long-term outcomes after external beam irradiation and brachytherapy boost for base-of-tongue cancers. Int J Radiat Oncol Biol Phys 57:489–494
Virtaniemi JA, Kumpulainen EJ, Hirvikoski PP, Johansson RT, Kosma VM (2001) The incidence and etiology of postlaryngectomy pharyngocutaneous fistulae. Head Neck 23:29–33
Paydarfar JA, Birkmeyer NJ (2006) Complications in head and neck surgery: a meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch Otolaryngol Head Neck Surg 132:67–72
Paderno A, Piazza C, Bresciani L, Vella R, Nicolai P (2016) Microvascular head and neck reconstruction after (chemo)radiation: facts and prejudices. Curr Opin Otolaryngol Head Neck Surg 24:83–90
Kwon D, Genden EM, de Bree R et al (2018) Overcoming wound complications in head and neck salvage surgery. Auris Nasus Larynx 45:1135–1142
Abouyared M, Kerr DA, Burroway B et al (2019) Abnormal microvasculature in laryngectomy mucosal margins may be associated with increased risk of fistula. Head Neck Pathol 13:364–370
Hui Y, Wei WI, Yuen PW, Lam LK, Ho WK (1996) Primary closure of pharyngeal remnant after total laryngectomy and partial pharyngectomy: how much residual mucosa is sufficient? Laryngoscope 106:490–494
Powell J, Ullal UR, Ahmed O, Ragbir M, Paleri V (2014) Tissue transfer to post-chemoradiation salvage laryngectomy defects to prevent pharyngocutaneous fistula: single-centre experience. J Laryngol Otol 128:1–3
Withrow KP, Rosenthal EL, Gourin CG et al (2007) Free tissue transfer to manage salvage laryngectomy defects after organ preservation failure. Laryngoscope 117:781–784
Patel UA, Moore BA, Wax M et al (2013) Impact of pharyngeal closure technique on fistula after salvage laryngectomy. JAMA Otolaryngol Head Neck Surg 139:1156–1162
Hanasono MM, Lin D, Wax MK, Rosenthal EL (2012) Closure of laryngectomy defects in the age of chemoradiation therapy. Head Neck 34:580–588
Petersen JF, Pezier TF, van Dieren JM et al (2019) Dilation after laryngectomy: incidence, risk factors and complications. Oral Oncol 91:107–112
Montgomery WW (1978) Salivary bypass tube. Ann Otol Rhinol Laryngol 87:159–162
Saydam L, Kalcioglu T, Kizilay A (2002) Early oral feeding following total laryngectomy. Am J Otolaryngol 23:277–281
Bondi S, Giordano L, Limardo P, Bussi M (2013) Role of Montgomery salivary stent placement during pharyngolaryngectomy, to prevent pharyngocutaneous fistula in high-risk patients. J Laryngol Otol 127:54–57
Kamhieh Y, Fox H, Hallett E, Berry S (2018) Routine use of salivary bypass tubes in laryngectomy patients: systematic review. J Laryngol Otol 132:380–384
Tabet JC, Johnson JT (1990) Wound infection in head and neck surgery: prophylaxis, etiology and management. J Otolaryngol 19:197–200
Rubin J, Johnson JT, Wagner RL, Yu VL (1988) Bacteriologic analysis of wound infection following major head and neck surgery. Arch Otolaryngol Head Neck Surg 114:969–972
Harris R, Ofo E, Cope D et al (2015) Current trends in antibiotic prophylaxis for laryngectomy in the UK—a national survey. J Laryngol Otol 129:63–67
Simo R, French G (2006) The use of prophylactic antibiotics in head and neck oncological surgery. Curr Opin Otolaryngol Head Neck Surg 14:55–61
Seven H, Sayin I, Turgut S (2004) Antibiotic prophylaxis in clean neck dissections. J Laryngol Otol 118:213–216
Jeannon JP, Orabi A, Manganaris A, Simo R (2010) Methicillin Resistant Staphylococcus Aureus Infection as a causative agent of fistula formation following total laryngectomy for advanced head & neck cancer. Head Neck Oncol 2:14
Busoni M, Deganello A, Gallo O (2015) Pharyngocutaneous fistula following total laryngectomy: analysis of risk factors, prognosis and treatment modalities. Acta Otorhinolaryngol Ital 35:400–405
Funding
This research received no external funding
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Data sharing statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Piazza, C., Paderno, A., Del Bon, F. et al. Fascio-cutaneous-free flaps as primary reconstruction in salvage total laryngectomy. Eur Arch Otorhinolaryngol 278, 219–226 (2021). https://doi.org/10.1007/s00405-020-06137-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06137-x