Abstract
Purpose
Most studies regarding residual and recurrent cholesteatoma focus on single relapse. This study examines patients who had to undergo at least three surgeries for complete eradication of their cholesteatoma, with the aim of bringing to light risk factors and assessing the functional impact of multiple surgeries on hearing.
Method
We include 27 patients who underwent 3 consecutive surgeries for cholesteatoma between 2006 and 2016. This population represented 3.1% of all cholesteatoma operated on during that same period (868 patients).
Results
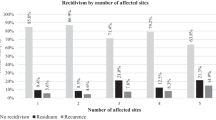
Cases of multi-residual and/or recurrent cholesteatoma (RRC) were significantly younger (13.1 years old), than single-RRC or cases with No-RRC (respectively, 28.0 and 38.5 years old) (p < 0.01). Furthermore, there was a significant difference in cholesteatoma location especially for combined attical and mesotympanic location between the three groups (no-RCC 26%; single-RRC 34% and multi-RRC 66%) (p < 0.01). There was also a significant difference in ossicular erosion of the malleus, incus and stapes between the three groups (p < 0.01). In our study, the type of surgery did not influence multi-RRC rates. We did not observe any significant impact on hearing between the first and third surgeries. Mean duration between the first and second surgeries was significantly shorter for multi-RRC (14.5 months SD 8.3) than for single-RRC (23.3 months SD 18.1) (p < 0.05).
Conclusion
Special care should be given in case of combined attical and mesotympanic extension, ossicular erosion and young children. Delaying the realization of MRI, and/or of second-look surgery, could decrease the risk of multi-RRC.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Vartiainen E (1995) Factors associated with recurrence of cholesteatoma. J Laryngol Otol 109:590–592
Roger G, Denoyelle F, Chauvin P et al (1997) Predictive risk factors of residual cholesteatoma in children: a study of 256 cases. Am J Otol 18:550–558
Ahn S-H, Oh SH, Chang SO, Kim C-S (2003) Prognostic factors of recidivism in pediatric cholesteatoma surgery. Int J Pediatr Otorhinolaryngol 67:1325–1330
Britze A, Møller ML, Ovesen T (2017) Incidence, 10-year recidivism rate and prognostic factors for cholesteatoma. J Laryngol Otol 131:319–328. https://doi.org/10.1017/S0022215117000299
Iino Y, Imamura Y, Kojima C et al (1998) Risk factors for recurrent and residual cholesteatoma in children determined by second stage operation. Int J Pediatr Otorhinolaryngol 46:57–65
Kerckhoffs KGP, Kommer MBJ, van Strien THL et al (2016) The disease recurrence rate after the canal wall up or canal wall down technique in adults. Laryngoscope 126:980–987. https://doi.org/10.1002/lary.25591
Tomlin J, Chang D, McCutcheon B, Harris J (2013) Surgical technique and recurrence in cholesteatoma: a meta-analysis. Audiol Neurootol 18:135–142. https://doi.org/10.1159/000346140
Kuo C-L, Liao W-H, Shiao A-S (2015) A review of current progress in acquired cholesteatoma management. Eur Arch Otorhinolaryngol 272:3601–3609. https://doi.org/10.1007/s00405-014-3291-0
Muzaffar J, Metcalfe C, Colley S, Coulson C (2017) Diffusion-weighted magnetic resonance imaging for residual and recurrent cholesteatoma: a systematic review and meta-analysis. Clin Otolaryngol 42:536–543. https://doi.org/10.1111/coa.12762
Bazzi K, Wong E, Jufas N, Patel N (2019) Diffusion-weighted magnetic resonance imaging in the detection of residual and recurrent cholesteatoma in children: a systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol 118:90–96. https://doi.org/10.1016/j.ijporl.2018.12.031
(1995) Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. AmericanAcademy of Otolaryngology-Head and Neck Surgery Ffoundation, Inc. Otolaryngol Head Neck Surg 113:186–187. https://doi.org/10.1016/S0194-5998(95)70103-6
Clark JG (1981) Uses and abuses of hearing loss classification. ASHA 23:493–500
Parisier SC, Hanson MB, Han JC et al (1996) Pediatric cholesteatoma: an individualized, single-stage approach. Otolaryngol-Head Neck Surg 115:107–114. https://doi.org/10.1016/S0194-5998(96)70145-6
Wetmore RF, Konkle DF, Potsic WP, Handler SD (1987) Cholesteatoma in the pediatric patient. Int J Pediatr Otorhinolaryngol 14:101–112
Gristwood RE, Venables WN (1990) Factors influencing the probability of residual cholesteatoma. Ann Otol Rhinol Laryngol 99:120–123
Stangerup SE, Drozdziewicz D, Tos M (1999) Cholesteatoma in children, predictors and calculation of recurrence rates. Int J Pediatr Otorhinolaryngol 49(Suppl 1):S69–73
Prasad SC, La Melia C, Medina M et al (2014) Long-term surgical and functional outcomes of the intact canal wall technique for middle ear cholesteatoma in the paediatric population. Acta Otorhinolaryngol Ital 34:354–361
Kemppainen HO, Puhakka HJ, Laippala PJ et al (1999) Epidemiology and aetiology of middle ear cholesteatoma. Acta Otolaryngol (Stockh) 119:568–572
Gaillardin L, Lescanne E, Morinière S et al (2012) Residual cholesteatoma: prevalence and location. Follow-up strategy in adults. Eur Ann Otorhinolaryngol Head Neck Dis 129:136–140. https://doi.org/10.1016/j.anorl.2011.01.009
Presutti L, Gioacchini FM, Alicandri-Ciufelli M et al (2014) Results of endoscopic middle ear surgery for cholesteatoma treatment: a systematic review. Acta Otorhinolaryngol Ital Organo Uff Della Soc Ital Otorinolaringol E Chir Cerv-facc 34:153–157
Killeen DE, Tolisano AM, Kou YF et al (2019) Recidivism after endoscopic treatment of cholesteatoma. Otol Neurotol 40:1313–1321. https://doi.org/10.1097/MAO.0000000000002395
Lecler A, Lenoir M, Peron J et al (2015) Magnetic resonance imaging at one year for detection of postoperative residual cholesteatoma in children: is it too early? Int J Pediatr Otorhinolaryngol 79:1268–1274. https://doi.org/10.1016/j.ijporl.2015.05.028
Tos M, Lau T (1989) Late results of surgery in different cholesteatoma types. ORL J Oto-Rhino-Laryngol Relat Spec 51:33–49
Rosenfeld RM, Moura RL, Bluestone CD (1992) Predictors of residual-recurrent cholesteatoma in children. Arch Otolaryngol Head Neck Surg 118:384–391
Acknowledgements
We would like to thank all the patients who participated in this study. We would also like to thank all the surgeons who contributed to this study, especially Dr. Sonia Ayari-Khalfallah. Finally we would like to thank Dr. Margaux Grall for helping with the writing of the manuscript and Dr. Gunther Huyghues des Etages for helping with data collection.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declare any conflict of interest.
Ethical approval
This study complies with the ethical and legal requirements of the French law (March 5, 2012) and the Declaration of Helsinki. Approval from the Ethics comity of the Lyon University Hospital was received for this study (no. 20-05).
Informed consent
In accordance with French law (March 5, 2012) with regards to research limited to gathering retrospective data stemming from medical files, all patients were informed that they had the right to refuse that their data or information be used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hermann, R., Blanc, J., Fieux, M. et al. Multi-operated cholesteatoma: when two surgeries are not enough. Eur Arch Otorhinolaryngol 278, 665–673 (2021). https://doi.org/10.1007/s00405-020-06104-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06104-6