Abstract
Objective
Lateral and central compartments cervical lymph nodes metastases are common among patients with papillary thyroid carcinoma (PTC). Elective level VI neck dissection during thyroidectomy and lateral neck dissection (LND) for the treatment of PTC with lateral compartment lymph node metastases is controversial because of the uncertain benefit in clinical outcomes and increased risks of surgical morbidity.
We aimed to determine the potential benefit of elective level VI neck dissection in patients with cN1 papillary thyroid carcinoma (PTC) by investigating the rate and pattern of locoregional recurrence in PTC patients who underwent total thyroidectomy and therapeutic lateral node dissection (LND; levels II–IV) without elective level VI dissection.
Methods
A retrospective cohort study. Data on demographics, clinical presentation and workup, intraoperative and pathological report, postoperative course, adjuvant therapy, recurrence patterns, and overall survival were retrieved from the medical charts of patients who underwent thyroid surgery in our hospital between January 2006 and December 2017.
Results
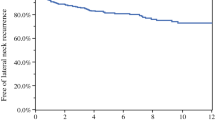
A total of 1415 thyroidectomies were performed during the study period, of which 802 (56.67%) were for PTC. Of those PTC patients, 228 (28.42%) also underwent LND (levels II–VI) during the same thyroidectomy procedure. Thirty-four (14.91%) of those 228 patients, underwent total thyroidectomy with therapeutic lateral ND II–IV without elective level VI ND. During the follow-up period, five (14.7%) of the latter cohort were diagnosed with recurrence in central neck (level VI) lymph nodes, and four of them (11.7%) were diagnosed with ipsilateral recurrence at level VI.
Conclusion
Our results revealed 11.7% rate of clinically significant recurrent disease in ipsilateral level VI which, in our opinion, does not justify routine prophylactic level VI ND dissection when the ipsilateral lateral neck is operated for metastases.


Similar content being viewed by others
Change history
13 August 2020
The original article can be found online.
Abbreviations
- ATA:
-
American Thyroid Association
- LND:
-
Lateral neck dissection
- MCI:
-
Millicurie
- ND:
-
Neck dissection
- PTC:
-
Papillary thyroid carcinoma
- RA:
-
Radioiodine ablation
- TASMC:
-
Tel Aviv Sourasky Medical Center
- TG:
-
Thyroglobulin
- US:
-
Ultrasound
- WDTC:
-
Well-differentiated thyroid carcinoma
References
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
Cady B et al (1976) Changing clinical, pathologic, therapeutic, and survival patterns in differentiated thyroid carcinoma. Ann Surg 184:541–553
Wada N et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas. Ann Surg 237:399–407
Yan D et al (2011) Cervical lymph node metastasis in clinical N0 papillary thyroid carcinoma. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 46:887–891
Degroot LJ, Kaplan EL, McCormick M, Straus FH (1990) Natural history, treatment, and course of papillary thyroid carcinoma*. J Clin Endocrinol Metab 71:414–424
Sellers M et al (1992) Prognostic significance of cervical lymph node metastases in differentiated thyroid cancer. Am J Surg 164:578–581
Mazzaferri EL, Young RL, Oertel JE, Kemmerer WT, Page CP (1977) Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine (Baltimore) 56:171–196
Cady B, Rossi R (1988) An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery 104:947–953
Hay ID, McConahey WM, Goellner JR (2002) Managing patients with papillary thyroid carcinoma: insights gained from the Mayo Clinic’s experience of treating 2512 consecutive patients during 1940 through 2000. Trans Am Clin Climatol Assoc 113:241–260
Mazzaferri EL, Young RL (1981) Papillary thyroid carcinoma: a 10 year foliow-up report of the impact of therapy in 576 patients. Am J Med 70:511–518
Rossi RL, Cady B, Silverman ML, Wool MS, Horner TA (1986) Current results of conservative surgery for differentiated thyroid carcinoma. World J Surg 10:612–621
Asimakopoulos P, Nixon IJ, Shaha AR (2017) Differentiated and medullary thyroid cancer: surgical management of cervical lymph nodes. Clin Oncol 29:283–289
Tollefsen HR, Shah JP, Huvos AG (1972) Papillary carcinoma of the thyroid Recurrence in the thyroid gland after initial surgical treatment. Am J Surg 124:468–472
Haugen BR et al. (2015) American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26 (2016).
Hughes CJ, Shaha AR, Shah JP, Loree TR (1996) Impact of lymph node metastasis in differentiated carcinoma of the thyroid: a matched-pair analysis. Head Neck 18:127–132
Shaha AR, Shah JP, Loree TR (1996) Risk group stratification and prognostic factors in papillary carcinoma of thyroid. Ann Surg Oncol 3:534–538
Stulak JM et al (2006) Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 141:489
Kouvaraki MA et al (2003) Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery 134:946–954 (discussion 954-5)
Sadowski BM, Snyder SK, Lairmore TC (2009) Routine bilateral central lymph node clearance for papillary thyroid cancer. Surgery 146:696–705
Shaha AR (2009) Prophylactic central compartment dissection in thyroid cancer: a new avenue of debate. Surgery 146:1224–1227
Hughes DT et al (2010) Influence of prophylactic central lymph node dissection on postoperative thyroglobulin levels and radioiodine treatment in papillary thyroid cancer. Surgery 148:1100–1107
Randolph GW et al (2012) The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid 22:1144–1152
Pereira JA et al (2005) Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery 138:1095–1101
Giordano D et al (2012) Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 22:911–917
Roh JL, Kim JM, Park C II (2011) Central lymph node metastasis of unilateral papillary thyroid carcinoma: patterns and factors predictive of nodal metastasis, morbidity, and recurrence. Ann Surg Oncol 18:2245–2250
Goropoulos A et al (2004) Value of the cervical compartments in the surgical treatment of papillary thyroid carcinoma. World J Surg 28:1275–1281
Khafif A et al (2008) Elective paratracheal neck dissection for lateral metastases from papillary carcinoma of the thyroid: is it indicated? Head Neck 30:306–310
Qu H, Sun G, Liu Y, He Q (2015) Clinical risk factors for central lymph node metastasis in papillary thyroid carcinoma: a systematic review and meta-analysis. Clin Endocrinol (Oxf) 83:124–132
Liang J, Li Z, Fang F, Yu T, Li S (2017) Is prophylactic central neck dissection necessary for cN0 differentiated thyroid cancer patients at initial treatment? A meta-analysis of the literature. Acta Otorhinolaryngol Ital 37:1–8
Nixon IJ et al (2013) Observation of clinically negative central compartment lymph nodes in papillary thyroid carcinoma. Surgery 154:1166–1173
Hartl DM et al (2012) Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg 255:777–783
Zetoune T et al (2010) Prophylactic central neck dissection and local recurrence in papillary thyroid cancer: a meta-analysis. Ann Surg Oncol 17:3287–3293
Cooper DS et al (2009) Revised American thyroid association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Agrawal N et al (2017) Indications and extent of central neck dissection for papillary thyroid cancer: an American head and neck society consensus statement. Head Neck 39:1269–1279
Carling T et al (2012) American thyroid association design and feasibility of a prospective randomized controlled trial of prophylactic central lymph node dissection for papillary thyroid carcinoma. Thyroid 22:237–244
Koo BS, Choi EC, Park Y-H, Kim E-H, Lim YC (2010) Occult contralateral central lymph node metastases in papillary thyroid carcinoma with unilateral lymph node metastasis in the lateral neck. J Am Coll Surg 210:895–900
Shindo ML et al (2014) Management of invasive well-differentiated thyroid cancer: an American head and neck society consensus statement: AHNS consensus statement. Head Neck n/a-n/a. https://doi.org/10.1002/hed.23619
Trivizki O, Amit M, Fliss DM, Gil Z (2013) Elective central compartment neck dissection in patients with papillary thyroid carcinoma recurrence. Laryngoscope 123:1564–1568
Acknowledgement
Ester Eshkol is thanked for her editorial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to declare.
Ethical approval
Retrospective cohort study, IBR approved 704-16TLV.
Human and animal rights
Research does not involve human participants and/or animals.
Informed consent
Informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised due to one of the author name was incorrect and corrected in this version.
Rights and permissions
About this article
Cite this article
Carmel-Neiderman, N.N., Duek, I., Amsterdam, D. et al. Total thyroidectomy with therapeutic level II–IV neck dissection for papillary thyroid carcinoma: level VI recurrence patterns. Eur Arch Otorhinolaryngol 277, 3449–3455 (2020). https://doi.org/10.1007/s00405-020-06079-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06079-4