Abstract
Objective
White matter lesions (WMLs) are the most common central nervous system changes observed during cochlear implant evaluation. However, its clinical significance in cochlear implantation (CI) remains unclear. The purpose of this study is to explore the effects of WMLs on hearing and speech rehabilitation of prelingually deaf children after CI.
Methods
The data of forty-five children with WMLs who received CI from 2011 to 2014 were retrospectively reviewed. All patients underwent magnetic resonance imaging examination preoperatively. The categories of auditory performance (CAP) and speech intelligibility rating (SIR) scales were used to evaluate changes in the auditory and speech abilities of the patients, and the Fazekas scale was adopted to assess the extent of WMLs. The degree of WMLs was divided into four grades (none, mild, moderate, severe). We assessed hearing and speech abilities at the following time points: 6, 12, 24, 36, 48 and 60-months post-operation.
Results
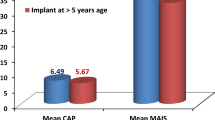
No significant differences in CAP scores were observed between WMLs groups and the control group at 12 months post-CI (p = 0.099), but marked between-group differences were found at 6, 24, 48- and 60-months post-CI. (p < 0.05). Similarly, no significant differences in the SIR scores were observed at 6 months post-CI (p = 0.087), but marked between-group differences were found at 12, 24, 48- and 60- months post-CI. (p < 0.05). Analysis of stratified group results revealed improvements in hearing and speech development for all the subgroups, including the severe WMLs subgroup following CI. However, hearing and speech ability of the severe WMLs subgroup was much slower than that of other groups.
Conclusions
The auditory and speech abilities of prelingually deaf children with WMLs and those without WMLs can improve after CI. Therefore, WMLs should not be considered a contraindication for CI. However, the decision to perform CI in such patients needs a comprehensive evaluation because the post-surgery effects on children with severe WMLs are not ideal.




Similar content being viewed by others
References
Wilson BS, Tucci DL, Merson MH, O'Donoghue GM (2017) Global hearing health care: new findings and perspectives. The Lancet 390(10111):2503–2515. https://doi.org/10.1016/S0140-6736(17)31073-5
Hong P, Jurkowski ZC, Carvalho DS (2010) Preoperative cerebral magnetic resonance imaging and white matter changes in pediatric cochlear implant recipients. Int J Pediatr Otorhinolaryngol 74(6):658–660. https://doi.org/10.1016/j.ijporl.2010.03.014
Jonas NE, Ahmed J, Grainger J, Jephson CG, Wyatt ME, Hartley BE, Saunders D, Cochrane LA (2012) MRI brain abnormalities in cochlear implant candidates: How common and how important are they? Int J Pediatr Otorhinolaryngol 76(7):927–929. https://doi.org/10.1016/j.ijporl.2012.02.070
Lapointe A, Viamonte C, Morriss MC, Manolidis S (2006) Central nervous system findings by magnetic resonance in children with profound sensorineural hearing loss. Int J Pediatr Otorhinolaryngol 70(5):863–868. https://doi.org/10.1016/j.ijporl.2005.09.022
Young JY, Ryan ME, Young NM (2014) Preoperative imaging of sensorineural hearing loss in pediatric candidates for cochlear implantation. Radiographics Rev Publ Radiol Soc N Am Inc 34(5):133–149. https://doi.org/10.1148/rg.345130083
Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE (2006) Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med 355(7):685–694. https://doi.org/10.1056/NEJMoa053792
Iwata S, Nakamura T, Hizume E, Kihara H, Takashima S, Matsuishi T, Iwata O (2012) Qualitative brain MRI at term and cognitive outcomes at 9 years after very preterm birth. Pediatrics 129(5):e1138–1147. https://doi.org/10.1542/peds.2011-1735
Moon IJ, Kim EY, Park G-Y, Jang MS, Kim JH, Lee J, Chung W-H, Cho Y-S, Hong SH (2012) The clinical significance of preoperative brain magnetic resonance imaging in pediatric cochlear implant recipients. Audiol Neurotol 17(6):373–380. https://doi.org/10.1159/000341818
Xu X-Q, Wu F-Y, Hu H, Su G-Y, Shen J (2015) Incidence of Brain Abnormalities Detected on Preoperative brain MR imaging and their effect on the outcome of cochlear implantation in children with sensorineural hearing loss. Int J Biomed Imaging 2015:6. https://doi.org/10.1155/2015/275786
Luthra S, Nagarkar A (2010) 1418 Leukodystrophy & its effects on rehabilitation of children with cochlear implant: a preliminary case study. Pediatr Res 68(1):701–701. https://doi.org/10.1203/00006450-201011001-01418
Archbold S, Lutman ME, Nikolopoulos T (1998) Categories of auditory performance: inter-user reliability. Br J Audiol 32(1):7–12. https://doi.org/10.3109/03005364000000045
Allen MC, Nikolopoulos TP, O'Donoghue GM (1998) Speech intelligibility in children after cochlear implanation. Otol Neurotol 19(6):742–746
Fazekas F, Chawluk J, Alavi A, Hurtig H, Zimmerman R (1987) MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging. Am J Roentgenol 149(2):351–356
Smith RJH, Bale JF, White KR (2005) Sensorineural hearing loss in children. The Lancet 365(9462):879–890. https://doi.org/10.1016/S0140-6736(05)71047-3
Davis A, Wood S (1992) The epidemiology of childhood hearing impairment: factor relevant to planning of services. Br J Audiol 26(2):77–90. https://doi.org/10.3109/03005369209077875
Fortnum HM, Marshall DH, Summerfield AQ (2002) Epidemiology of the UK population of hearing-impaired children, including characteristics of those with and without cochlear implants–audiology, aetiology, comorbidity and affluence. Int J Audiol 41(3):170–179. https://doi.org/10.3109/14992020209077181
van Beeck Calkoen EA, Sanchez Aliaga E, Merkus P, Smit CF, van de Kamp JM, Mulder MF, Goverts ST, Hensen EF (2017) High prevalence of abnormalities on CT and MR imaging in children with unilateral sensorineural hearing loss irrespective of age or degree of hearing loss. Int J Pediatr Otorhinolaryngol 97:185–191. https://doi.org/10.1016/j.ijporl.2017.04.002
Collins SE, Spencer-Smith M, Mürner-Lavanchy I, Kelly CE, Pyman P, Pascoe L, Cheong J, Doyle LW, Thompson DK, Anderson PJ (2019) White matter microstructure correlates with mathematics but not word reading performance in 13-year-old children born very preterm and full-term. NeuroImage Clin 24:101944. https://doi.org/10.1016/j.nicl.2019.101944
Inder TE, Warfield SK, Wang H, Hüppi PS, Volpe JJ (2005) Abnormal cerebral structure is present at term in premature infants. Pediatrics 115(2):286–294. https://doi.org/10.1542/peds.2004-0326
Woodward LJ, Clark CAC, Bora S, Inder TE (2012) Neonatal white matter abnormalities an important predictor of neurocognitive outcome for very preterm children. PLoS ONE 7(12):e51879. https://doi.org/10.1371/journal.pone.0051879
Vickers D, De Raeve L, Graham J (2016) International survey of cochlear implant candidacy. Cochlear Implants Int 17(sup1):36–41. https://doi.org/10.1080/14670100.2016.1155809
Levi-montalcini R (1949) The development of the acoustico-vestibular centres in the chick embryo in the absence of the afferent root fibers and of descending fiber tracts. J Comp Neurol 91(2):209–241. https://doi.org/10.1002/cne.900910204
Matthews MR, Powell TP (1962) Some observations on transneuronal cell degeneration in the olfactory bulb of the rabbit. J Anat 96:89–102
Westenbroek RE, Westrum LE, Hendrickson AE, Wu JY (1988) Ultrastructure of synaptic remodeling in piriform cortex of adult rats after neonatal olfactory bulb removal: an immunocytochemical study. J Comp Neurol 274(3):334–346. https://doi.org/10.1002/cne.902740304
Ryugo DK, Kretzmer EA, Niparko JK (2005) Restoration of auditory nerve synapses in cats by cochlear implants. Science (New York, NY) 310(5753):1490–1492. https://doi.org/10.1126/science.1119419
Ryugo DK, Rosenbaum BT, Kim PJ, Niparko JK, Saada AA (1998) Single unit recordings in the auditory nerve of congenitally deaf white cats: morphological correlates in the cochlea and cochlear nucleus. J Comp Neurol 397(4):532–548. https://doi.org/10.1002/(sici)1096-9861(19980810)397:4%3c532:aid-cne6%3e3.0.co;2-2
CM F (2012) The behavioral neurology of white matter, 2nd edn. Oxford University Press, New York
Funding
This study was supported by funding from the project of the Anhui Provincial Education Department and Boston scientific (No.9021082201).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors have read and approved the manuscript and have no conflict of interest of this paper.
Informed consent
Approval for this study was obtained from the local ethics committee of The First Affiliated Hospital of Anhui Medical University, Hefei, Anhui, P.R. China. Written informed consent of both parents to the patients was obtained before the study. All data were collected and analyzed retrospectively.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, S., Zheng, W., Li, H. et al. Cochlear implantation in prelingually deaf children with white matter lesions. Eur Arch Otorhinolaryngol 278, 323–329 (2021). https://doi.org/10.1007/s00405-020-06075-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06075-8