Abstract
Background/objective
An adult with vocal fold nodules can suffer from hoarseness, breathiness and vocal fatigue, which, in turn, significantly affects their vocal participation as well as activities. A well-designed voice therapy program improves the quality of life and vocal functionality. This is a narrative review with a systematic search of the current literature about the effectiveness of voice therapy interventions in adults with vocal fold nodules.
Methods
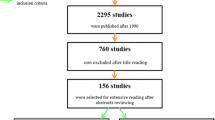
Several key terms were used for the database electronic search of articles. Strict inclusion criteria were used and a broad evaluation of the studies was performed. This included the level of evidence based on the National Health and Medical Research Council levels of evidence, assessment, and critical appraisal.
Results
Nine out of 30 reviewed articles met the criteria of inclusion and reported positive effects of voice therapy intervention on adult patients with vocal fold nodules. The vast majority of the reviewed studies reported multidimensional voice measures outcome data, most of them containing visual-perceptual, auditory-perceptual, acoustic and self-assessment results. Regardless of receiving direct or indirect or a combination of both voice therapy contents, nearly all voice quality parameters were found to improve after treatment. Short-term treatment (< 3 weeks) may be as beneficial as longer traditional voice therapy programs, and using telepractice voice therapy may be an achievable and practical way of delivering treatment and enhance adherence to therapy. The study design and the evidence levels of the included studies were low (≤ III-2) and the risk of bias of the comparative studies was moderate.
Conclusion
This narrative review cannot conclude the general effectiveness of voice therapy programs. Further research and understanding of what specific parameters (exercise and techniques) of a therapy’s content will improve voice outcome measures. More studies are required to investigate whether or not voice therapy benefits are sustainable 6 months after ending the therapy. However, improved evidence is required to suggest that short period treatments are as beneficial as traditional therapy programs. Telepractice voice therapy may be an achievable and practical way of delivering treatment and enhance adherence to therapy.


Similar content being viewed by others
References
Kunduk M, McWhorter AJ (2009) True vocal fold nodules: the role of differential diagnosis. Curr Opin Otolaryngol Head Neck Surg 17:449–452. https://doi.org/10.1097/MOO.0b013e3283328b6d
Pedersen M, McGlashan J (2012) Surgical versus non-surgical interventions for vocal cord nodules. Cochrane Database Syst Rev 2012(6):CD001934. https://doi.org/10.1002/14651858.CD001934.pub2
Rosen CA, Gartner-Schmidt J, Hathaway B et al (2012) A nomenclature paradigm for benign midmembranous vocal fold lesions. Laryngoscope 122:1335–1341. https://doi.org/10.1002/lary.22421
Birchall MA, Carding P (2019) Vocal nodules management. Clin Otolaryngol 44:497–501
Van Houtte E, Van Lierde K, D’Haeseleer E, Claeys S (2010) The prevalence of laryngeal pathology in a treatment-seeking population with dysphonia. Laryngoscope 120:306–312. https://doi.org/10.1002/lary.20696
Coyle SM, Weinrich BD, Stemple JC (2001) Shifts in relative prevalence of laryngeal pathology in a treatment-seeking population. J Voice 15:424–440
Zhukhovitskaya A, Battaglia D, Khosla SM et al (2015) Gender and age in benign vocal fold lesions. Laryngoscope 125:191–196. https://doi.org/10.1002/lary.24911
Casper JK, Leonard R (2006) Understanding voice problems: a physiological perspective for diagnosis and treatment. Lippincott Williams & Wilkins, Philadelphia
Tae K, Kim KY, Yun BR et al (2012) Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc 26:1871–1877. https://doi.org/10.1007/s00464-011-2116-0
Vilkman E (2000) Voice problems at work: a challenge for occupational safety and health arrangement. Folia Phoniatr Logop 52:120–125
Jones K, Sigmon J, Hock L et al (2002) Prevalence and risk factors for voice problems among telemarketers. Arch Otolaryngol Neck Surg 128:571–577
Chernobelsky SI (2007) The treatment and results of voice therapy amongst professional classical singers with vocal fold nodules. Logop Phoniatr Vocology 32:178–184
Syed I, Daniels E, Bleach NR (2009) Hoarse voice in adults: an evidence-based approach to the 12 minute consultation. Clin Otolaryngol 34:54–58. https://doi.org/10.1111/j.1749-4486.2008.01872.x
Hsiung M-W, Hsiao Y-C (2004) The characteristic features of muscle tension dysphonia before and after surgery in benign lesions of the vocal fold. ORL 66:246–254
Nelson R, Gray SD, Simon M, Dove H (2001) An evaluation of the effects of two treatment approaches for teachers with voice disorders: a prospective randomized clinical trial. J Speech Lang Hear Res 44:286
Pedersen M, Beranova A, Møller S (2004) Dysphonia: medical treatment and a medical voice hygiene advice approach. A prospective randomised pilot study. Eur Arch Oto Rhino Laryngol Head Neck 261:312–315
Stemple JC (2005) A holistic approach to voice therapy. In: Seminars in speech and language. Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, pp 131–137
Stemple JC, Roy N, Klaben BK (2018) Clinical voice pathology: theory and management. Plural Publishing, San Diego
Warren SF, Fey ME, Yoder PJ (2007) Differential treatment intensity research: a missing link to creating optimally effective communication interventions. Ment Retard Dev Disabil Res Rev 13:70–77
Chagnon F, Stone RE (1996) Nodules and polyps. In: Brown WS Jr, Vinson BP, Crary MA (eds) Organic voice disorders: assessment and treatment. Singular Publishing Group Inc, San Diego
Pannbacker M (1999) Treatment of vocal nodules: options and outcomes. Am J Speech Lang Pathol 8:209–217
National Health Medical Research Council (2009) NHMRC additional levels of evidence and grades for recommendations for developers of guidelines. National Health Medical Research Council, Canberra
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Sterne JAC, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Fu S, Theodoros DG, Ward EC (2015) Delivery of intensive voice therapy for vocal fold nodules via telepractice: a pilot feasibility and efficacy study. J Voice 29:696–706. https://doi.org/10.1016/j.jvoice.2014.12.003
Fu S, Theodoros D, Ward EC (2016) Long-term effects of an intensive voice treatment for vocal fold nodules. Int J Speech Lang Pathol 18:77–88. https://doi.org/10.3109/17549507.2015.1081286
Fu S, Theodoros DG, Ward EC (2015) Intensive versus traditional voice therapy for vocal nodules: perceptual, physiological, acoustic and aerodynamic changes. J Voice 29:260.e31–260.e44. https://doi.org/10.1016/j.jvoice.2014.06.005
Mashima PA, Birkmire-Peters DP, Syms MJ et al (2003) Telehealth: voice therapy using telecommunications technology. Am J Speech Lang Pathol 12:32–39
Holmberg EB, Doyle P, Perkell JS et al (2003) Aerodynamic and acoustic voice measurements of patients with vocal nodules: variation in baseline and changes across voice therapy. J Voice 17:269–282
Lucchini E, Maccarini AR, Bissoni E et al (2018) Voice improvement in patients with functional dysphonia treated with the proprioceptive-elastic (PROEL) method. J Voice 32:209–215
Khoramshahi H, Khatoonabadi AR, Khoddami SM et al (2018) Responsiveness of Persian version of consensus auditory perceptual evaluation of voice (CAPE-V), Persian version of voice handicap index (VHI), and Praat in vocal mass lesions with muscle tension dysphonia. J Voice 32:770-e21
Chhetri SS, Gautam R (2015) Acoustic analysis before and after voice therapy for laryngeal pathology. Kathmandu Univ Med J 13:323–327
Verdolini-Marston K, Burke MK, Lessac A et al (1995) Preliminary study of two methods of treatment for laryngeal nodules. J Voice 9:74–85
de Oliveira Santos JK, Silverio KCA, Diniz Oliveira NFC, Gama ACC (2016) Evaluation of electrostimulation effect in women with vocal nodules. J Voice 30:769.e1–769.e7. https://doi.org/10.1016/j.jvoice.2015.10.023
Dejonckere PH (2000) Clinical implementation of a multidimensional basic protocol for assessing functional results of voice therapy. A preliminary study. Rev Laryngol 121:311–313
Carding PN, Steen IN, Webb A et al (2004) The reliability and sensitivity to change of acoustic measures of voice quality. Clin Otolaryngol Allied Sci 29:538–544
Pring T (2005) Research methods in communication disorders. Wiley, New York
Robey RR (2004) A five-phase model for clinical-outcome research. J Commun Disord 37:401–411
Cherney LR (2012) Aphasia treatment: intensity, dose parameters, and script training. Int J Speech Lang Pathol 14:424–431
Hart T, Tsaousides T, Zanca JM, Whyte J, Packel A, Ferraro M, Dijkers MP (2014) Toward a theory-driven classification of rehabilitation treatments. Arch Phys Med Rehabil 95(1):S33–S44
Jani R, Jaana S, Laura L, Jos V (2008) Systematic review of the treatment of functional dysphonia and prevention of voice disorders. Otolaryngol Neck Surg 138(5):557–565
Van Stan JH, Roy N, Awan S et al (2015) A taxonomy of voice therapy. Am J Speech Lang Pathol 24:101–125
Togher L (2012) Challenges inherent in optimizing speech-language pathology outcomes: it’s not just about counting the hours. Int J Speech Lang Pathol 14:438–442
Kamhi AG (2012) Pharmacological dosage concepts: how useful are they for educators and speech-language pathologists? Int J Speech Lang Pathol 14:414–418
Roy N (2012) Optimal dose–response relationships in voice therapy. Int J Speech Lang Pathol 14:419–423
Enderby P (2012) How much therapy is enough? The impossible question! Int J Speech Lang Pathol 14:432–437
Yoder P, Fey ME, Warren SF (2012) Studying the impact of intensity is important but complicated. Int J Speech Lang Pathol 14:410–413
Schmitt MB, Justice LM (2012) Optimal intervention intensity for emergent literacy: what we know and need to learn. Int J Speech Lang Pathol 14:451–455
Barsties v. Latoszek B, Ulozaitė-Stanienė N, Petrauskas T et al (2019) Diagnostic accuracy of dysphonia classification of DSI and AVQI. Laryngoscope 129:692–698
Uloza V, Latoszek BBV, Ulozaite-Staniene N et al (2018) A comparison of Dysphonia Severity Index and Acoustic Voice Quality Index measures in differentiating normal and dysphonic voices. Eur Arch Oto Rhino Laryngol 275:949–958
Wuyts FL, De Bodt MS, Molenberghs G et al (2000) The Dysphonia Severity Index: an objective measure of vocal quality based on a multiparameter approach. J Speech Lang Hear Res 4300:796–809. https://doi.org/10.1044/jslhr.4303.796
Acknowledgements
The last author acknowledges the support of FP-ENAS.
Funding
This study was not funded by any company or any other source of funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable as the article is a Systematic Search and Narrative Review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alegria, R., Vaz Freitas, S. & Manso, M.C. Effectiveness of voice therapy in patients with vocal fold nodules: a systematic search and narrative review. Eur Arch Otorhinolaryngol 277, 2951–2966 (2020). https://doi.org/10.1007/s00405-020-06059-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06059-8