Abstract
Objective
We aimed to analyze the results of 24-h multichannel intraluminal impedance and pH-monitoring (MII-pH) of the laryngopharynx and esophagus in asymptomatic volunteers. Moreover, we also aimed to gain insight into and establish a baseline for laryngopharyngeal reflux in the healthy population by quantitatively and qualitatively comparing the reflux and pH distribution in both the laryngopharynx and the esophagus.
Methods
Healthy volunteers were recruited and observed; they underwent 24-h ambulatory combined MII-pH monitoring. The proximal sensor (pH1) was positioned approximately 1 cm above the upper esophageal sphincter with the aid of a solid-state high-resolution esophageal manometer. Laryngopharyngeal reflux events were detected and characterized by the incidence and property of reflux both in the laryngopharynx and the esophagus.
Results
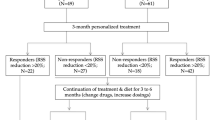
Thirty-eight asymptomatic volunteers who completed all the examinations were included in this study. The median pH detected by the proximal sensor was 6.6 (6.2, 7.0), with an average of 6.58 ± 0.74. A total of 814 laryngopharyngeal reflux events were detected, including 722 (89%) in the upright position and 92 (11%) in the supine position with incidence (0%) in the liquid state, 44 (5%) in the mixture, and 769 (95%) in the gaseous state. Furthermore, 5 incidences (1%) of acid reflux and 809 incidences of non-acid reflux (99%) were noted. A total of 5779 esophageal reflux events were detected, including 5020 (87%) in the upright position, 759 (13%) in the supine position, with 2051 (36%) in the liquid state, 2050 (35%) in the mixed condition, and 1678 (29%) in the gaseous state; adding up to 805 incidences (14%) of acid reflux and 4974 incidences (86%) of non-acid reflux.
Conclusion
Non-acid reflux in the upright position is characteristic of laryngopharyngeal reflux. Acid reflux is almost undetectable in healthy subjects. Hence, the diagnostic indicators of gastroesophageal reflux disease are not suitable for laryngopharyngeal reflux disease.









Similar content being viewed by others
References
Lechien JR, Akst LM, Hamdan AL et al (2019) Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Head Neck Surg 160(5):762–782
Koufman JA, Aviv JE, Casiano RR, Shaw GY et al (2002) Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg 127(1):32–35
Qu Y, Ye J (2015) Laryngopharyngeal reflux disease. Chin ENT News Rev 3:142–145
Pace F, Annese V, Ceccatelli P et al (2000) Ambulatory oesophageal pH-metry. Position paper of the Working Team on Oesophageal pH-metry by the GISMAD (Gruppo Italiano di Studio sulla Motilita dell'Apparato Digerente). Dig Liver Dis 32(4):357–436
Muderris T, Gokcan MK, Yorulmaz I et al (2009) The clinical value of pharyngeal pH monitoring using a double-probe, triple-sensor catheter in patients with laryngopharyngeal reflux. Arch Otolaryngol Head Neck Surg 135(2):163–167
Belafsky PC, Postma GN, Koufman JA et al (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16:274–277
Belafsky PC, Postma GN, Koufman JA et al (2001) The Validity and reliability of the Reflux Finding Score (RFS). Laryngoscope 111:1313–1317
Lee JS, Jung AR, Park JM et al (2018) Comparison of characteristics according to reflux type in patients with laryngopharyngeal reflux. Clin Exp Otorhinolaryngol. 11(2):141–145
Harrell SP, Koopman J, Woosley S et al (2007) Exclusion of pH artifacts is essential for hypopharyngeal pH monitoring. Laryngoscope 117(3):470–474
Xiao YL, Lin JK, Cheung TK et al (2009) Normal values of 24-hour combined esophageal multichannel intraluminal impedance and pH monitoring in the Chinese population. Digestion 79(2):109–114
Shay S, Tutuian R, Sifrim D et al (2004) Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol 99(6):1037
Balaji NS, Blom D, Demeester TR et al (2003) Redefining gastroesophageal reflux (GER). Surg Endosc 17(9):1380
Zentilin P, Iiritano E, Dulbecco P et al (2006) Normal values of 24-h ambulatory intraluminalimpedance combined with pH-metry in subjects eating a Mediterranean diet. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver 38(4):226
Zerbib F, Varannes SBD, Roman S et al (2005) Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian-French cohort of healthy subjects. Aliment Pharmacol Ther 22(10):1011–1021
Maldonado A, Diederich L, Castell DO et al (2003) Laryngopharyngeal reflux identified using a new catheter design: defining normal values and excluding artifacts. Laryngoscope 113(2):349–355
Shaker R, Milbrath M, Ren J et al (1995) Esophagopharyngeal distribution of refluxed gastric acid in patients with reflux laryngitis. Gastroenterology 109(5):1575–1582
Bove M, Ruth M, Cange L et al (2000) 24-H pharyngeal pH monitoring in healthy volunteers: a normative study. Scand J Gastroenterol 35(3):234–241
Borges LF, Chan WW, Carroll TL (2018) Dual pH probes without proximal esophageal and pharyngeal impedance may be deficient in diagnosing LPR. J Voice 33:697–703
Zhang R, Li X, Wang L et al (2013) Esophageal dynamic and laryngopharyngeal reflux play a role in pathogenesis of vocal cord polyps. Chin J Otorhinolaryngol Head Neck Surg 48(06):455–460
Muderris T, Gokcan MK, Yorulmaz I et al (2009) The Clinical value of pharyngeal ph monitoring using a double-probe, triple-sensor catheter in patients with laryngopharyngeal reflux. Arch Otolaryngol Head Neck Surg 135(2):163–167
Wang AJ, Liang MJ, Jiang AY et al (2011) Gastroesophageal and laryngopharyngeal reflux detected by 24-hour combined impedance and pH monitoring in healthy Chinese volunteers. J Dig Dis 12(3):173
Hoppo T, Sanz AF, Nason KS et al (2012) How Much pharyngeal exposure is “Normal”? Normative data for laryngopharyngeal reflux events using hypopharyngeal multichannel intraluminal impedance (HMII). J Gastrointest Surg 16(1):16–25
Luebke K, Samuels TL, Chelius TH et al (2017) Pepsin as a biomarker for laryngopharyngeal reflux in children with laryngomalacia. Laryngoscope 127(10):2413–2417
Chander B, Hanley-Williams N, Deng Y et al (2012) 24 versus 48-hour Bravo pH monitoring. J Clin Gastroenterol 46(3):197–200
Francis DO, Patel DA, Sharda R et al (2016) Patient-reported outcome measures related to laryngopharyngeal reflux: a systematic review of instrument development and validation. Otolaryngol Head Neck Surg 155(6):923–935
Lechien JR, Bobin F, Muls V (2020) Validity and reliability of the reflux symptom score. Laryngoscope 130(3):E98–E107
Kavookjian H, Irwin T, Garnett JD et al (2020) The reflux symptom index and symptom overlap in dysphonic patients. Laryngoscope 6:1–6
Lechien JR, Schindler A, De Marrez LG et al (2019) Instruments evaluating the clinical findings of laryngopharyngeal reflux: a systematic review [J]. Laryngoscope 129(3):720–736
Chang BA et al (2015) The reliability of the reflux finding score among general otolaryngologists. J Voice 29:572–577
Milstein CF, Charbel S, Hicks DM et al (2005) Prevalence of laryngeal irritation signs associated with reflux in asymptomatic volunteers: impact of endoscopic technique (rigid vs. flexible laryngoscope). Laryngoscope 115(12):2256–2261
Qi Z, Zhang Y, Su R et al (2020) The influence of age on the score of reflux symptom index scale and reflux finding score scale in the diagnosis of pharyngeal and laryngeal reflux. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 34(2):170–172
Chen M, Hou C, Chen T et al (2018) Reflux symptom index and reflux finding score in 91 asymptomatic volunteers. Acta Otolaryngol 138(7):1–5
Smit CF, Mathus-Vliegen LMH, Van Leeuwen JAMJ et al (2003) Monitoring of laryngopharyngeal reflux: influence of meals and beverages. Ann Otol Rhinol Laryngol 112(2):109–112
Zhonggao W, Xiang G, Yungang L et al (2011) Phenomenon of pharynx Nozzle and 3S: an experimental study on gastroesophago-airway reflux. Clin Misdiagn Misther 24(3):5–7
Marcin SM, Benjamin WR, James CI et al (2011) Mechanisms of esophago-pharyngeal acid regurgitation in human subjects. PLoS One 6(7):e22630
Koufman JA (2002) Laryngopharyngeal reflux 2002: a new paradigm of airway disease. Ear Nose Throat J 81(2):2–6
Koufman JA (2002) Laryngopharyngeal reflux is different from classic gastroesophageal reflux disease. Ear Nose Throat J 81(9 Suppl 2):7–9
Fox M, Menne D, Stutz B et al (2006) The effects of tegaserod on oesophageal function and bolus transport in healthy volunteers: studies using concurrent high-resolution manometry and videofluoroscopy. Aliment Pharmacol Ther 24(7):1017–1027
Samuels TL, Johnston N (2009) Pepsin as a causal agent of inflammation during nonacidic reflux. Otolaryngol Head Neck Surg 141(3):559–563
Johnston N, Knight J, Dettmar PW et al (2004) Pepsin and carbonic anhydrase isoenzyme III as diagnostic markers for laryngopharyngeal reflux disease. Laryngoscope 114(12):2129–2134
Koufman JA (2011) Low-acid diet for recalcitrant laryngopharyngeal reflux: therapeutic benefits and their implications. Ann Otol Rhinol Laryngol 120(5):281
Wood JM, Hussey DJ, Woods CM et al (2011) Biomarkers and laryngopharyngeal reflux. J Laryngol Otol 125(12):1218
Musser J, Kelchner L, Neils-Strunjas J et al (2011) A comparison of rating scales used in the diagnosis of extraesophageal reflux. J Voice 25(3):293–300
Johnston N, Yan JC, Hoekzema CR et al (2012) Pepsin promotes proliferation of laryngeal and pharyngeal epithelial cells. Laryngoscope 122(6):1317–1325
Johnston N, Wells CW, Samuels TL et al (2009) Pepsin in nonacidic refluxate can damage hypopharyngeal epithelial cells. Ann Otol Rhinol Laryngol 118(9):677–685
Amarasiri DL, Pathmeswaran A, Silva HJD et al (2013) Response of the airways and autonomic nervous system to acid perfusion of the esophagus in patients with asthma: a laboratory study. BMC Pulm Med 13(1):33
Sataloff RT, Hawkshaw MJ, Gupta R (2010) Laryngopharyngeal reflux and voice disorders: an overview on disease mechanisms, treatments, and research advances. Discov Med 10(52):213–224
Jaspersen DM et al (2003) Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Alimentary Pharmacol Ther 17:1515–1520
Lechien JR, Bobin F, Muls V et al (2019) Gastroesophageal reflux in laryngopharyngeal reflux patients: clinical features and therapeutic response. Laryngoscope. https://doi.org/10.1002/lary.28482
Koufman JA (2002) Laryngopharyngeal reflux is different from classic gastroesophageal reflux disease. Ear Nose Throat J 81(9 Suppl 2):7–9
Wang L, Wang G, Li L (2020) Relationship between laryngopharyngeal reflux disease and gastroesophageal reflux diseasebased on synchronous esophageal and oropharyngeal Dx-pH monitoring. Am J Otolaryngol 24:102441
Koufman JA, Aviv JE, Casiano RR et al (2002) Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg 127(1):32–35
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
The study supported by the High-level hospital foster grants from Fujian Province Hospital, Fujian province, China (Grant number: 2019HSJJ13), 2018 Fujian Medical University Qihang Fund Project (Grant number: 2018OH1157), the National Natural Science Foundation of China (Grant no. 81970899) and supported by the training project of Fujian Province's health research talents Fund Project (Grant number: 2019-2-32).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest statement to disclose.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (include name of committee + reference number) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee of Fujian Provincial Hospital (Ethical approval number: K-2015–019-01).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hou, C., Chen, M., Chen, T. et al. Study on laryngopharyngeal and esophageal reflux characteristics using 24-h multichannel intraluminal impedance-pH monitoring in healthy volunteers. Eur Arch Otorhinolaryngol 277, 2801–2811 (2020). https://doi.org/10.1007/s00405-020-05969-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-05969-x