Abstract
Purpose
It has been shown that the reflux of the gastric content to the proximal oesophagus influences incidence of voice prosthesis (VP) complications in laryngectomized patients. We conducted prospective randomised study to investigate the relationship between pepsin concentration in saliva and occurrence of VP complications before and after 3 months of proton pump inhibitor (PPI) therapy.
Methods
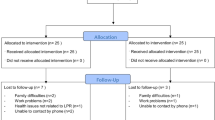
60 laryngectomized patients with VP and 30 controls were included in the study. Saliva samples were collected in the morning and concentration of pepsin were measured by Human Pepsin (PG) ELISA kit. Thirty-Four (57%) patients reported one or more VP complication and were randomised in two groups, with and without PPI therapy, 40 mg pantoprazole per day for 3 months.
Results
Patients who had longer time since last VP change had higher incidence of periprosthetic and transprosthetic leakage and Candida colonisation. Pepsin was found in all saliva samples. Median saliva pepsin concentration level did not significantly differ between laryngectomized patients and control subjects, or between patients with and without VP complications, and there was no correlation between saliva pepsin concentration levels and type of VP complication. After 3 months therapy, there was no difference in median saliva pepsin level or incidence of VP complication between patients with and without PPI therapy.
Conclusion
Although reflux was proposed to be associated with VP complications and pepsin was proven as a most sensitive and specific marker of EER, we did not find any statistically significant correlation between pepsin levels and occurrence of VP complications. A 3 months 40 mg pantoprazole therapy was ineffective in reduction of VP complications in our study group.




Similar content being viewed by others
References
Barbiera F, Fiorentino E, Lo Greco V, Galia M, Musto GA, Runza G, Sorrentino F, Sparacia G, Lo CA (2003) Digital cineradiography of the pharynx and the oesophagus after total or partial laryngectomy. Radiol Med 106:169–177
Choi EC, Hong WP, Kim CB, Yoon HC, Nam JI, Son EJ, Kim KM, Kim SH (2003) Changes of esophageal motility after total laryngectomy. Otolaryngol Head Neck Surg 128:691–699
Kuhnt T, Jirsak N, Müller AC, Pelz T, Gernhardt C, Schaller HG, Janich M, Gerlach R, Dunst J (2005) Quantitative and qualitative investigations of salivary gland function in dependence on irradiation dose and volume for reduction of xerostomia in patients with head-and-neck cancer. Strahlenther Onkol 181:520–528
Izdebski K, Fontanesi J, Ross JC, Hetzler D (1988) The effects of irradiation on alaryngeal voice of totally laryngectomized patients. Int J Radiat Oncol Biol Phys 14:1281–1286
Lorenz KJ, Grieser L, Ehrhart T, Maier H (2010) Role of reflux in tracheoesophageal fistula problems after laryngectomy. Ann Otol Rhinol Laryngol 119:719–728
Lorenz KJ, Kraft K, Graf F, Pröpper C, Steinestel K (2015) Importance of cellular tight junction complexes in the development of periprosthetic leakage after prosthetic voice rehabilitation. HNO 63(3):171–172
Lorenz KJ, Kraft K, Graf F, Pröpper C, Steinestel K (2015) Role of reflux-induced epithelial-mesenchymal transition in periprosthetic leakage after prosthetic voice rehabilitation. Head Neck 37(4):530–536
Pattani KM, Morgan M, Nathan CO (2009) Reflux as a cause of tracheoesophageal puncture failure. Laryngoscope 119:121–125
Cocuzza S, Bonfiglio M, Chiaramonte R, Aprile G, Mistretta A, Grosso G, Serra A (2012) Gastroesophageal reflux disease and postlaryngectomy tracheoesophageal fistula. Eur Arch Otorhinolaryngol 269:1483–1488
Samuels TL, Johnston N (2010) Pepsin as a marker of extraesophageal reflux. Ann Otol Rhinol Laryngol 119:203–208
Calvo-Henríquez C, Ruano-Ravina A, Vaamonde P, Martínez-Capoccioni G, Martín-Martín C (2017) Is pepsin a reliable marker of laryngopharyngeal reflux? A systematic review. Otolaryngol Head Neck Surg 157(3):385–391
Wang J, Zhao Y, Ren J, Xu Y (2018) Pepsin in saliva as a diagnostic biomarker in laryngopharyngeal reflux: a meta-analysis. Eur Arch Otorhinolaryngol. 275(3):671–678
Bock JM, Brawley MK, Johnston N, Samuels T, Massey BL, Campbell BH, Toohill RJ, Blumin JH (2010) Analysis of pepsin in tracheoesophageal puncture sites. Ann Otol Rhinol Laryngol 119:799–805
de Coul BO, Hilgers F, Balm A, Tan I, van den Hoogen F, van Tinteren H (2000) A decade of postlaryngectomy vocal rehabilitation in 318 patients: a single Institutions experience with consistent application of provox indwelling voice prostheses. Arch Otolaryngol Head Neck Surg 126:1320–1328
Lukinović J, Bilić M, Raguž I, Živković T, Kovač-Bilić L, Prgomet D (2012) Overview of 100 patients with voice prosthesis after total laryngectomy—experience of single institution. Coll Antropol 36:99–102
Malik T, Bruce I, Cherry J (2007) Surgical complications of tracheo-oesophageal puncture and speech valves. Curr Opin Otolaryngol Head Neck Surg 15:117–122
Acton LM, Ross DA, Sasaki CT, Leder SB (2008) Investigation of tracheoesophageal voice prosthesis leakage patterns: patient’s self report versus clinician’s confirmation. Head Neck 30:618–621
Hilgers FJ, Balm AJ (1993) Long-term results of vocal rehabilitation after total laryngectomy with the low-resistance, indwelling Provox voice prosthesis system. Clin Otolaryngol Allied Sci 18:517–523
Hutcheson KA, Lewin JS, Sturgis EM, Risser J (2012) Multivariable analysis of risk factors for enlargement of the tracheoesophageal puncture after total laryngectomy. Head Neck 34:557–567
Boscolo-Rizzo P, Marchiori C, Gava A, Da Mosto MC (2008) The impact of radiotherapy and GERD on in situ lifetime of indwelling voice prostheses. Eur Arch Otorhinolaryngol 265:791–796
Hutcheson KA, Lewin JS, Sturgis EM, Kapadia A, Risser J (2011) Enlarged tracheoesophageal puncture after total laryngectomy: a systematic review and meta-analysis. Head Neck 33:20–30
de Carpentier JP, Ryder WD, Saeed SR, Woolford TJ (1996) Survival times of Provox valves. J Laryngol Otol 110:37–42
Delsupehe K, Zink I, Lejaegere M, Delaere P (1998) Prospective randomized comparative study of tracheoesophageal voice prosthesis: Blom-Singer versus Provox. Laryngoscope 108:1561–1565
Sifrim D, Castell D, Dent J, Kahrilas PJ (2004) Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut 53:1024–1031
Andersson O, Ylitalo R, Finizia C, Bove M, Magnus R (2006) Pharyngeal reflux episodes at pH 5 in healthy volunteers. Scand J Gastroenterol 41:138–143
Vaezi MF, Schroeder PL, Richter JE (1997) Reproducibility of proximal probe pH parameters in 24-h ambulatory esophageal pH monitoring. Am J Gastroenterol 92:825–829
Hirano I, Richter JE (2007) ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol 102:668–685
Oelschlager BK, Quiroga E, Isch JA, Cuenca-Abente F (2006) Gastroesophageal and pharyngeal reflux detection using impedance and 24-hour pH monitoring in asymptomatic subjects: defining the normal environment. J Gastrointest Surg 10:54–62
Na SY, Kwon OE, Lee YC, Eun YG (2016) Optimal timing of saliva collection to detect pepsin in patients with laryngopharyngeal reflux. Laryngoscope 126(12):2770–2773
Lechien JR, Akst LM, Hamdan AL, Schindler A, Karkos PD, Barillari MR, Calvo-Henriquez C, Crevier-Buchman L, Finck C, Eun YG, Saussez S, Vaezi MF (2019) Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Head Neck Surg 160(5):762–782
Acknowledgements
We would like to express our special thanks of gratitude to Robert Tičac, MD, Dijana Pedisić Maržić, MD, Marija Pastorčić Grgić,MD,PhD, Pavle Perše, MD, Tomislav Tomičević, MD, Assist. Prof. Željko Zubčić, MD, PhD and Tamara Živković, SLP, for help during patient inclusion in study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal participant statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of the University of Zagreb, ethics committee of General Hospital Dr. Josip Bencevic, Clinical Hospital Centre Zagreb, Clinical Hospital Centre Rijeka, Clinical Hospital Centre Osijek, and Clinical Hospital Centre Sestre Milosrdnice, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Danic Hadzibegovic, A., Kozmar, A., Hadzibegovic, I. et al. Influence of proton pump inhibitor therapy on occurrence of voice prosthesis complications. Eur Arch Otorhinolaryngol 277, 1177–1184 (2020). https://doi.org/10.1007/s00405-020-05784-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-05784-4