Abstract
Purpose
In the rare case of intractable, posterior, non-sphenopalatine artery epistaxis, ligation of ethmoidal arteries using an external approach like a Lynch-type incision is required. Orbital complications, especially extra-ocular motility disorders with diplopia, are known, but in the literature rarely described. Our aim was to analyse the complication type, rate, and outcome of ethmoidal artery ligation for epistaxis.
Materials and methods
Data between 2012 and 2017 of patients treated with ethmoidal artery ligation were analysed retrospectively and through a telephone interview using a non-standardized questionnaire.
Results
Data of 18 patients (m/f = 3/15) aged 53–83 years were reviewed. Epistaxis recurred in only one patient after 1 month. Five patients (28%) suffered from diplopia shortly after surgery. Motility analysis revealed full recovery with free motility in four out of five reported cases after 4–8 months, one patient still reports intermittent mild diplopia more than 1 year postoperatively.
Conclusion
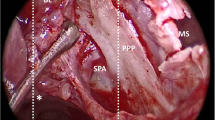
In patients with intractable, non-sphenopalatine artery epistaxis, anterior ethmoidal artery ligation was highly effective. Diplopia, however, occurred in one-third of our patient group. Information about motility restriction with longer standing diplopia are mandatory when consenting patients for ligation of ethmoidal arteries. Special care needs to be taken during dissection in the region of the trochlea and superior oblique muscle.
Level of evidence: Case Series, level 4



Similar content being viewed by others
References
Small M, Murray JA, Maran AG (1982) A study of patients with epistaxis requiring admission to hospital. Health Bull (Edinb). 40(1):20–29
Varshney S, Saxena RK (2005) Epistaxis: A retrospective clinical study. Indian J Otolaryngol Head Neck Surg. 57(2):125–129
Klotz DA, Winkle MR, Richmon J, Hengerer AS (2002) Surgical management of posterior epistaxis: a changing paradigm. Laryngoscope. 112(9):1577–1582
de Bonnecaze G, Gallois Y, Chaynes P, Bonneville F, Dupret-Bories A, Chantalat E et al (2017) Intractable epistaxis: which arteries are responsible? An angiographic study. Surg Radiol Anat. 39(11):1203–1207
Kindler RM, Holzmann D, Landis BN, Ditzen B, Soyka MB (2016) The high rate of long-term recurrences and sequelae after epistaxis treatment. Auris Nasus Larynx 43(4):412–417
Umapathy N, Quadri A, Skinner DW (2005) Persistent epistaxis: what is the best practice? Rhinology. 43(4):305–308
Kahn A, Laccourreye L, Fournier HD, Brecheteau C (2017) Ptosis and vertical diplopia after ligation of ethmoidal arteries. J Stomatol Oral Maxillofac Surg. 118(2):129–131
Yeh S, Yen MT, Foroozan R (2004) Orbital apex syndrome after ethmoidal artery ligation for recurrent epistaxis. Ophthal Plast Reconstr Surg. 20(5):392–394
Couch JM, Somers ME, Gonzalez C (1990) Superior oblique muscle dysfunction following anterior ethmoidal artery ligation for epistaxis. Arch Ophthalmol. 108(8):1110–1113
Christmann LM, Wolin MJ (1991) Superior oblique palsy as a complication of anterior ethmoidal artery ligation. Arch Ophthalmol. 109(6):767
Murer K, Holzmann D, Burkhardt JK, Soyka MB (2015) An unusual complication of epistaxis: cerebral abscess formation after anterior ethmoidal artery ligation. BMJ Case Rep. https://doi.org/10.1136/bcr-2015-213389
Douglas SA, Gupta D (2003) Endoscopic assisted external approach anterior ethmoidal artery ligation for the management of epistaxis. J Laryngol Otol 117(2):132–133
Turri-Zanoni M, Arosio AD, Stamm AC, Battaglia P, Salzano G, Romano A et al (2018) Septal branches of the anterior ethmoidal artery: anatomical considerations and clinical implications in the management of refractory epistaxis. Eur Arch Otorhinolaryngol 275(6):1449–1456
Sokoloff J, Wickbom I, McDonald D, Brahme F, Goergen TC, Goldberger LE (1974) Therapeutic percutaneous embolization in intractable epistaxis. Radiology 111(2):285–287
Floreani S, Nair S, Switajewski M, Wormald P (2006) Endoscopic anterior ethmoidal artery ligation: a cadaver study. Laryngoscope 116(7):1263–1267
Erdogmus S, Govsa F (2006) The anatomic landmarks of ethmoidal arteries for the surgical approaches. J Craniofac Surg 17(2):280–285
Camp AA, Dutton JM, Caldarelli DD (2009) Endoscopic transnasal transethmoid ligation of the anterior ethmoid artery. Am J Rhinol Allergy 23(2):200–202
Simmen D, Raghavan U, Briner HR, Manestar M, Schuknecht B, Groscurth P et al (2006) The surgeon's view of the anterior ethmoid artery. Clin Otolaryngol 31(3):187–191
Kimmelman CP, Weisman RA, Osguthorpe JD, Kay SL (1988) The efficacy and safety of transantral ethmoidectomy. Laryngoscope. 98(11):1178–1182
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial conflicts of interest to disclose.
Ethical approval
Patients who were interviewed by telephone gave oral consent to participate in the study; for the retrospective data collection, consent was waived by the ethical committee.
Research involving human participants and/or animals
This research involves human participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.



Rights and permissions
About this article
Cite this article
Bischoff, S., Gerth-Kahlert, C., Holzmann, D. et al. Longstanding diplopia after ethmoidal artery ligation for epistaxis. Eur Arch Otorhinolaryngol 277, 161–167 (2020). https://doi.org/10.1007/s00405-019-05686-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05686-0