Abstract
Purpose
To describe the procedures and investigate the hearing outcomes and complications after revision surgery for patients with otosclerosis in Sweden and compare these with previously published reports and to investigate factors that may predict the outcomes of revision surgery.
Methods
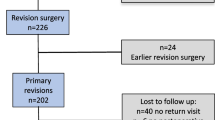
A total of 254 patients from the Swedish Quality Register for otosclerosis surgery who underwent surgery at 21 clinics were identified as having undergone revision surgery for otosclerosis from 2003 to 2013. Clinical records and audiograms from each of these patients were collected and analyzed.
Results
Improvement in hearing by 20 dB or more and closure of air–bone gap (≤ 20 dB) was achieved in 43% and 69% of patients after a first revision operation and in 46% and 70% of patients after a second revision operation. Most patients who underwent surgery because of dizziness were relieved of their dizziness. Postoperative deafness occurred in 2.3% of patients. Prior successful otosclerosis surgery predicted successful revision surgery, especially after a second revision operation. Fixation of the incus or malleus and finding of no obvious reason for the conductive hearing loss predicted a worse hearing outcome.
Conclusions
The hearing results after revision surgery in Sweden is somewhat inferior to those of previously published results involving large centers. Postoperative deafness may be as much as fivefold more common after revision surgery than after primary surgery. Meticulous reading of previous charts and honest counseling regarding the risks and expectations is mandatory before planning revision surgery for otosclerosis.



Similar content being viewed by others
References
Skrivan J, Cada Z, Kluh J, Boucek J, Profant O, Betka J (2014) Revision operations after previous stapes surgery for persisting hearing loss. Bratisl Lek Listy 115(7):442–444
Albers AE, Schönfeld U, Kandilakis K, Jovanovic S (2013) CO2 laser revision stapedotomy. Laryngoscope 123(6):1519–1526
Stucken EZ, Brown KD, Selesnick SH (2012) The use of KTP laser in revision stapedectomy. Otol Neurotol 33(8):1297–1299
Thiel G, Mills R (2011) Persistent and recurrent conductive deafness following stapedotomy. J Laryngol Otol 125(5):460–466
Bakhos D, Lescanne E, Charretier C, Robier A (2010) A review of 89 revision stapes surgeries for otosclerosis. Eur Ann Otorhinolaryngol Head Neck Dis 127(5):177–182
Vincent R, Rovers M, Zingade N, Oates J, Sperling N, Devèze A, Grolman W (2010) Revision stapedotomy: operative findings and hearing results. A prospective study of 652 cases from the Otology-Neurotology Database. Otol Neurotol 31(6):875–882
Babighian GG, Albu S (2009) Failures in stapedotomy for otosclerosis. Otolaryngol - Head Neck Surg 141(3):395–400
Mangham CA (2009) Long-term impact of incus necrosis on revision stapes surgery: incus versus malleus reconstruction. Otol Neurotol 30(8):1145–1151
Schmid P, Häusler R (2009) Revision stapedectomy: an analysis of 201 operations. Otol Neurotol 30(8):1092–1100
Gros A, Vatovec J, Zargi M, Jenko K (2005) Success rate in revision stapes surgery for otosclerosis. Otol Neurotol 26(6):1143–1148
Puxeddu R, Ledda GP, Pelagatti CL, Salis G, Puxeddu P (2005) Revision stapes surgery for recurrent transmissional hearing loss after stapedectomy and stapedotomy for otosclerosis. Acta Otorhinolaryngol Ital organo Uff della Soc Ital di Otorinolaringol e Chir cervico-facciale 25(6):347–352
Kohan D, Sorin A (2003) Revision stapes surgery: the malleus to oval window wire-piston technique. Laryngoscope 113(9):1520–1524
Lippy WH, Battista RA, Berenholz L, Schuring AG, Burkey JM (2003) Twenty-year review of revision stapedectomy. Otol Neurotol 24(4):560–566
De La Cruz A, Fayad JN (2000) Revision stapedectomy. Otolaryngol Head Neck Surg 123(6):728–732
Hammerschlag PE, Fishman A, Scheer AA (1998) A review of 308 cases of revision stapedectomy. Laryngoscope 108(12):1794–1800
Shea JJ (1998) Forty years of stapes surgery. Am J Otol 19:52–55
Han WW, Incesulu A, McKenna MJ, Rauch SD, Nadol JB, Glynn RJ (1997) Revision stapedectomy: intraoperative findings, results, and review of the literature. Laryngoscope 107(9):1185–1192
Magliulo G, Cristofari P, Terranova G (1997) Functional hearing results in revision stapes surgery. Am J Otol 18(4):408–412
Somers T, Govaerts P, de Varebeke SJ, Offeciers E (1997) Revision stapes surgery. J Laryngol Otol 111(3):233–239
Battista RA, Wiet RJ, Joy J (2006) Revision Stapedectomy. Otolaryngol Clin. North 39(4):677–697
Pauli NP, Strömbäck K, Lundman L, Dahlin-Redfors Y (2019) Surgical technique in stapedotomy hearing outcome and complications. Laryngoscope. https://doi.org/10.1002/lary.28072
Strömbäck K, Lundman L, Bjorsne A, Grendin J, Stjernquist-Desatnik A, Dahlin-Redfors Y (2017) Stapes surgery in Sweden: evaluation of a national-based register. Eur Arch Oto-Rhino-Laryngology 274(6):2421–2427
Wegner I, Vincent R, Derks LSM, Rauh SP, Heymans MW, Stegeman I, Grolman W (2018) An internally validated prognostic model for success in revision stapes surgery for tosclerosis. Laryngoscope 128:2390–2396
Lachance S, Bussières R, Côté M (2012) Stapes surgery in profound hearing loss due to otosclerosis. Otolo Neurotol 33:721–723
Merkus P, van LOON MC, Smit CF, Smits C, de Cock AF, Hensen EF (2011) Decision making in advanced otosclerosis: an evidence-based strategy. Laryngoscope 121:1935–1941
Mangam CA (2009) Long-term impact of incus necrosis on revision stapes surgery: incus versus malleus reconstruction. Otol Neurotol 30:1145–1151
Rambouesek A, Schlegel CH, Linder TE (2012) From incus bypass to malleostapedotomy: technical improvements and results. J Laryngol Otol 126(10):995–1002
Whetstone J, Nguyen A, Nguyen-Huynh A, Hamilton BE (2014) Surgical and clinical confirmation of temporal bone CT findings in patients with otosclerosis with failed stapes surgery. Head Neck 35(6), 1195–120129. Guyot J-P, Sakbani K (2007) Patients’ lives following stapedectomy complications. Adv Otorhinolaryngol 65:348–352
Ramaswamy AT, Lustig LR (2018) Revision surgery for otosclerosis. Otolaryngol Clin North Am 51:463–474
Acknowledgement
Jan Eklund, Centre of Registers Västra Götaland for statistical analysis.
Funding
This work was funded by the Swedish Association for Otorhinolaryngology Head Neck Surgery and the Center for Clinical Research in Värmland, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors are members of the professional committee that administrate the Swedish Quality Register for Otosclerosis Surgery (SQOS). Author Lars Lundman is also chairman for the National Quality Register for ENT-healthcare, in which SQOS is a part.
Informed consent
For this retrospective study spanning over a period of more than 1 decade, the Regional Ethics Committee in Uppsala, Sweden (ref. 2015/377) has approved collection of clinical data as described in the Materials and methods section, without written informed consent from each patient. The patients gave their informed consent to be registered in the SQOS database at the time of surgery and were then informed that the data could be used for clinical research in the future.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lundman, L., Strömbäck, K., Björsne, A. et al. Otosclerosis revision surgery in Sweden: hearing outcome, predictive factors and complications. Eur Arch Otorhinolaryngol 277, 19–29 (2020). https://doi.org/10.1007/s00405-019-05652-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05652-w