Abstract
Purpose
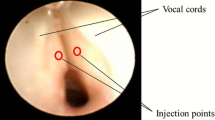
Surgical treatment is generally recommended for severe subglottic lesions following traumatic endotracheal intubation in children. An alternative approach is early transglottic corticosteroid administration to reduce scar formation and prevent the need for subsequent surgical intervention. This technique has been practiced successfully for several decades at the Children’s Hospital of Cologne and the outcomes of 26 subsequent patients reviewed in this analysis.
Methods
All patients who underwent transglottic corticosteroid injection for treatment of post-intubation stridor and dyspnoea between 2012 and 2018 were identified and their records and endoscopy images analysed. Severity of the endoscopic findings was assessed using the Myer–Cotton classification (MCC) and an Expected Need for Surgical Intervention (ENSI) score (1 = inevitable; 2 = very likely necessary; 3 = probably avoidable and 4 = most likely not necessary) was recorded. Treatment was considered successful if the children had a complete resolution of clinical symptoms.
Results
A total of 26 patients with a median (range) age of 1.9 (0.02–7.2) years and weight of 9.8 (1.8–25) kg were identified and included into the analysis. Endoscopic images were available for 22 children. All children underwent transglottic corticosteroid injection prior to any potential surgical treatment. A total of 22 patients (85%) improved following transglottic corticosteroid injection including 4 of 5 patients with a MCC = 3 and ENSI = 1 avoiding surgical intervention. None of the patients experienced a deterioration of clinical symptoms or endoscopic findings.
Conclusion
Transglottic corticosteroid injections as first-line treatment in children with severe post-endotracheal intubation trauma can successfully resolve symptoms and prevent invasive surgery.


Similar content being viewed by others
References
Sittel C (2012) Subglottic stenosis in the first year of life. Characteristics and treatment options. HNO 60(7):568–572. https://doi.org/10.1007/s00106-012-2508-z
Sittel C (2014) Pathologies of the larynx and trachea in childhood. Laryngorhinootologie 93(Suppl 1):S70–83. https://doi.org/10.1055/s-0033-1363212
Sittel C (2012) Paediatric laryngotracheal stenosis. Laryngorhinootologie 91(8):478–485. https://doi.org/10.1055/s-0032-1312629
Smith DF, de Alarcon A, Jefferson ND, Tabangin ME, Rutter MJ, Cotton RT, Hart CK (2018) Short- versus long-term stenting in children with subglottic stenosis undergoing laryngotracheal reconstruction. Otolaryngol Head Neck Surg 158(2):375–380. https://doi.org/10.1177/0194599817737757
Shabani S, Hoffman MR, Brand WT, Dailey SH (2017) Endoscopic management of idiopathic subglottic stenosis. Ann Otol Rhinol Laryngol 126(2):96–102. https://doi.org/10.1177/0003489416675357
Sharma SD, Gupta SL, Wyatt M, Albert D, Hartley B (2017) Safe balloon sizing for endoscopic dilatation of subglottic stenosis in children. J Laryngol Otol 131(3):268–272. https://doi.org/10.1017/s0022215117000081
Robles DT, Berg D (2007) Abnormal wound healing: keloids. Clin Dermatol 25(1):26–32. https://doi.org/10.1016/j.clindermatol.2006.09.009
Myer CM, O'Connor DM, Cotton RT (1994) Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol 103(4):319–323. https://doi.org/10.1177/000348949410300410
Smith RM, Rockoff MA (2011) CHAPTER 41—history of pediatric anesthesia. In: Cladis FP, Motoyama EK (eds) Smith's anesthesia for infants and children, 8th edn. Mosby, Philadelphia, pp 1294–1308. https://doi.org/10.1016/B978-0-323-06612-9.00041-9
Flagg PJ (1951) Endotracheal inhalation anesthesia. Special reference to postoperative reactions and suggestions for their elimination. Laryngoscope 61(8):818–831. https://doi.org/10.1288/00005537-195108000-00007
Tuft HS, Ratner SH (1947) Laryngeal polypoid granuloma following intratracheal anesthesia. Ann Otol Rhinol Laryngol 56(1):187–190
Baron SH, Kohlmoos HW (1951) Laryngeal sequelae of endotracheal anesthesia. Ann Otol Rhinol Laryngol 60(3):767–792. https://doi.org/10.1177/000348945106000320
Lampl L (2004) Tracheobronchial injuries. Conservative treatment. Interact Cardiovasc Thorac Surg 3(2):401–405. https://doi.org/10.1016/j.icvts.2004.02.016
Walner DL, Loewen MS, Kimura RE (2001) Neonatal subglottic stenosis–incidence and trends. Laryngoscope 111(1):48–51. https://doi.org/10.1097/00005537-200101000-00009
da Silva O, Stevens D (1999) Complications of airway management in very-low-birth-weight infants. Biol Neonate 75(1):40–45
Thomas RE, Rao SC, Minutillo C, Vijayasekaran S, Nathan EA (2017) Severe acquired subglottic stenosis in neonatal intensive care graduates: a case-control study. Arch Dis Child. https://doi.org/10.1136/archdischild-2017-312962
Schmidt AR, Weiss M, Engelhardt T (2014) The paediatric airway: basic principles and current developments. Eur J Anaesthesiol 31(6):293–299. https://doi.org/10.1097/eja.0000000000000023
Franco RA Jr, Husain I, Reder L, Paddle P (2017) Awake serial intralesional steroid injections without surgery as a novel targeted treatment for idiopathic subglottic stenosis. Laryngoscope. https://doi.org/10.1002/lary.26874
Wang CT, Lai MS, Cheng PW (2017) Long-term surveillance following intralesional steroid injection for benign vocal fold lesions. JAMA Otolaryngol Head Neck Surg 143(6):589–594. https://doi.org/10.1001/jamaoto.2016.4418
Yanagihara N, Azuma F, Koike Y, Honjo I, Imanishi Y (1964) Intracordal injection of dexamethasone. Pract Otorhinolaryngol 57:496–500
Hsu Y, Lan M, Chang S (2009) Percutaneous corticosteroid injection for vocal fold polyp. Arch Otolaryngol Head Neck Surg 135(8):776–780. https://doi.org/10.1001/archoto.2009.86
Cobb WB, Sudderth JF (1972) Intralesional steroids in laryngeal stenosis. A preliminary report. Arch Otolaryngol 96(1):52–56
Birck HG (1970) Endoscopic repair of laryngeal stenosis. Trans Am Acad Ophthalmol Otolaryngol 74(1):140–143
Othersen HB Jr (1974) The technique of intraluminal stenting and steroid administration in the treatment of tracheal stenosis in children. J Pediatr Surg 9(5):683–690
Massie RJ, Robertson CF, Berkowitz RG (2000) Long-term outcome of surgically treated acquired subglottic stenosis in infancy. Pediatr Pulmonol 30(2):125–130. https://doi.org/10.1002/1099-0496(200008)30:2%3c125:AID-PPUL7%3e3.0.CO;2-U
Acknowledgements
We discussed our observations with Hans L. J. Hoeve, MD, PhD, Rotterdam and thank him for his constructive contribution to our discussion.
Funding
No external funding was received for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human rights and animal participants
All procedures performed were in accordance with the ethical standards of the institutional research committee (waiver of formal ethical approval by Ethics Committee of University Witten/Herdecke, May 12th 2018 due to retrospective analysis with no personal data reported) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaufmann, J., Bode, K., Puder, C. et al. Transglottic corticosteroid injection for treatment of soft post-intubation subglottic stenosis: a retrospective analysis of 26 children. Eur Arch Otorhinolaryngol 276, 3419–3424 (2019). https://doi.org/10.1007/s00405-019-05642-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05642-y