Abstract
Objective
Post-tonsillectomy pain is one of the most frequent morbidities of tonsillectomy surgery. Currently, there is no standard protocol for post-tonsillectomy pain control. In our study, we aimed to compare the effects of perioperative peritonsillar dexamethasone–bupivacaine and bupivacaine-alone infiltration on pain control in pediatric patients.
Materials and methods
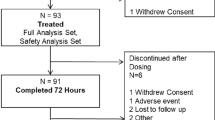
This prospective, randomized, double-blind, controlled clinical trial was conducted between February 2018 and May 2018 in a single-center tertiary education and research hospital, otorhinolaryngology/head and neck surgery clinic, under general anesthesia, which included 120 pediatric patients between the ages of 2–12 (mean 5.7 ± 1.8), and who were with ASA (American Society of Anesthesiologists) I–II classification. Patients were randomly divided into three groups as 40 participants in each group. Group 1 consisted of patients who were injected with dexamethasone–bupivacaine into their peritonsillar region, group 2 consisted of patients who were injected with bupivacaine only, and group 3 consisted of patients who were injected with saline only as the control group. FLACC (face, legs, activity, cry, consolability) Scale and Wong-Baker FACES® Pain Rating Scale (WBS) were used for early and late period postoperative pain scoring. Patients with pain score ≥ 4 were treated with paracetamol rescue analgesia. Side effects such as nausea, vomiting and bleeding were recorded. Data of all groups were compared statistically and p ≤ 0.05 was considered statistically significant.
Results
There was no significant difference between the groups in terms of demographic data, duration of operation and duration of anesthesia. The pain scores of group 1 were significantly lower than those of the control group except for postoperative 45th min, 2nd day and 3rd day. The pain scores of the group 1 were significantly lower at all times except for the postoperative 12th and 24th hour, than those of group 2. The pain scores of the group 2 were lower than the control group only at postoperative 7th day, but no significant difference was found at other times. No statistically significant difference was found between the groups in terms of requirement rates for the first 60 min recovery analgesia (p = 0.686). No statistical difference was found between the groups in terms of side effects.
Conclusion
In our study, preoperative local dexamethasone–bupivacaine infiltration in pediatric patients was shown to be more effective than bupivacaine-only and serum-only infiltration for early and late post-tonsillectomy pain control.



Similar content being viewed by others
References
Blacoe DA, Cunning E, Bell G (2008) Paediatric day-case surgery: an audit of unplanned hospital admission Royal Hospital for Sick Children, Glasgow. Anaesthesia 63:610–615
Ernst E, Fialka V (1994) Ice freezes pain? A review of the clinical effectiveness of analgesic cold therapy. J Pain Symptom Manag 9:56–59
Jebeles JA, Reilly JS, Gutierrez JF, Bradley EL Jr, Kissin I (1991) The effect of pre-incisional infiltration of tonsils with bupivacaine on the pain following tonsillectomy under general anesthesia. Pain 47:305–308
Anderson BJ, Ralph CJ, Stewart AW, Barber C, Holford NH (2000) The dose-effect relationship for morphine and vomiting after day-stay tonsillectomy in children. Anaesth Intensive Care 28:155–160
Heiba MH, Atef A, Mosleh M, Mohamed R, El-Hamamsy M (2012) Comparison of peritonsillar infiltration of tramadol and lidocaine for the relief of post-tonsillectomypain. J Laryngol Otol 126:1138–1141
Kimiaei-Asadi H, Nikooseresht M, Noori L, Behnoud F (2016) The effect of administration of ketamine and paracetamol versus paracetamol singly on post operative pain, nausea and vomiting after pediatric adenotonsillectomy. Anesth Pain Med 6(1):e31210. https://doi.org/10.5812/aapm.31210
Mattos JL, Robison JG, Greenberg J, Yellon RF (2014) Acetaminophen plus ibuprofen versus opioids for treatment of post-tonsillectomy pain in children. Int J Pediatr Otorhinolaryngol 78(10):1671–1676
El-Fattah AM, Ramzy EJ (2013) Pre-emptive triple analgesia protocol for tonsillectomy pain control in children: double-blind, randomised, controlled, clinical trial. J Laryngol Otol 127(4):383–391. https://doi.org/10.1017/S0022215113000364
Aouad MT, Siddik SS, Rizk LB, Zaytoun GM, Baraka AS (2001) The effect of dexamethasone on postoperative vomiting after tonsillectomy. Anesth Analg 92(3):636–640
Dostbil A, Celik M, Yoruk O, Ahmet AH, Fuat EA, Ilker I, Ali A (2014) Pre-emptive peritonsillar dexamethasone vs. levobupivacaine infiltration for relief of post-adenotonsillectomy pain in children: A controlled clinical study. Int J Pediatr Otorhinolaryngol 78(9):1467–1471. https://doi.org/10.1016/j.ijporl.2014.06.010
Huynh TM, Marret E, Bonnet F (2015) Combination of dexamethasone and local anaesthetic solution in peripheral nerve blocks: a meta-analysis of randomised controlled trials. Eur J Anaesthesiol 32(11):751–758. https://doi.org/10.1097/EJA.0000000000000248
Shafiei FT, Lopez J (2018) Bupivacaine. StatPearls Publishing, Treasure Island
Kaygusuz I, Susaman N (2003) The effects of dexamethasone, bupivacaine and topical lidocaine spray on pain after tonsillectomy. Int J Pediatr Otorhinolaryngol 67(7):737–742
Ju NY, Cui GX, Gao W (2013) Ropivacaine plus dexamethasone infiltration reduces postoperative pain after tonsillectomy and adenoidectomy. Int J Pediatr Otorhinolaryngol 77(11):1881–1885. https://doi.org/10.1016/j.ijporl.2013.08.037
Husband AD, Davis A (1996) Pain after tonsillectomy. Clin Otolaryngol 21(2):99–101
White PF (2008) Multimodal analgesia: its role in preventing postoperative pain. Curr Opin Investig Drugs 9(1):76–82 (review)
US Food and Drug Administration FDA (2014) Drug Safety Communication: safety review update of codeine use in children; new boxed warning and contraindication on use after tonsillectomy and/or adenoidectomy. US Food and Drug. http://www.fda.gov. Accessed 16 Jan 2017
Linxweiler M, Kühn JP, Wagner M, Al-Kadah B, Schick B (2018) Reduction of post-operative pain after tonsillectomy by a local mucosal flap—a prospective, randomized, controlled clinical trial on 100 adult patients. Acta Otolaryngol 138(10):913–920. https://doi.org/10.1080/00016489.2018.1497807
Kim JS, Kwon SH, Lee EJ, Yoon YJ (2017) Can intracapsular tonsillectomy be an alternative to classical tonsillectomy? A meta-analysis. Otolaryngol Head Neck Surg 157(2):178–189. https://doi.org/10.1177/0194599817700374
Molliex S, Haond P, Baylot D, Prades JM, Navez M, Elkhoury Z (1996) Effect of pre- vs. postoperative tonsillar infiltration with local anesthetics on postoperative pain after tonsillectomy. Acta Anaesthesiol Scand 40(10):1210–1215
Fedorowicz Z, van Zuuren EJ, Nasser M, Carter B, Al-Langawi JH (2013) Oral rinses, mouthwashes and sprays for improving recovery following tonsillectomy. Cochrane Database Syst Rev 10(9):CD007806. https://doi.org/10.1002/14651858
Cicekci F, Sizer C, Atici SS, Arican S, Karaibrahimoglu A, Kara I (2017) Comparison of the Perioperative and Postoperative effects of levobupivacaine and of levobupivacaine + adrenaline in pediatric tonsillectomy: a double-blind randomized study. Pain Res Manag 2017:8431823. https://doi.org/10.1155/2017/8431823
Sun J, Wu X, Meng Y, Jin L (2010) Bupivacaine versus normal saline for relief of post-adenotonsillectomy pain in children: a meta-analysis. Int J Pediatr Otorhinolaryngol 74(4):369–373. https://doi.org/10.1016/j.ijporl.2010.01.004
Bameshki AR, Razban M, Khadivi E, Razavi M, Bakhshaee M (2013) The effect of local injection of epinephrine and bupivacaine on post-tonsillectomy pain and bleeding. Iran J Otorhinolaryngol 5:209–214
Haytoğlu S, Arikan OK, Muluk NB, Kuran G (2015) Relief of pain at rest and during swallowing after modified cautery-assisted uvulopalatopharyngoplasty: bupivacaine versus lidocaine. J Craniofac Surg 26:216–223. https://doi.org/10.1097/SCS.0000000000001439
Steward DL, Grisel J, Meinzen-Derr J (2011) Steroids for improving recovery following tonsillectomy in children. Cochrane Database Syst Rev 10(8):CD003997. https://doi.org/10.1002/14651858
Movafegh A, Soroush AR, Navi A, Sadeghi M, Esfehani F, Akbarian-Tefaghi N (2007) The effect of intravenous administration of dexamethasone on postoperative pain, nausea, and vomiting after intrathecal injection of meperidine. Anesth Analg 104:987–989
Srinivasan B, Karnawat R, Mohammed S, Chaudhary B, Ratnawat A, Kothari SK (2016) Comparison of caudal and intravenous dexamethasone as adjuvants for caudal epidural block: a double blinded randomised controlled trial. Indian J Anaesth 60:948–954. https://doi.org/10.4103/0019-5049.195489
Desmet M, Vanneste B, Reynvoet M, Van Cauwelaert J, Verhelst L, Pottel H, Missant C, Van de Velde M (2015) A randomised controlled trial of intravenous dexamethasone combined with interscalene brachial plexus blockade for shoulder surgery. Anaesthesia 70:1180–1185
Huynh TM, Marret E, Bonnet F (2015) Combination of dexamethasone and local anaesthetic solution in peripheral nerve blocks: a meta-analysis of randomised controlled trials. Eur J Anaesthesiol 32:751–758. https://doi.org/10.1097/EJA.0000000000000248
Thimmasettaiah NB, Chandrappa RG (2012) A prospective study to compare the effects of pre, intra and post operative steroid (dexamethasone sodium phosphate) on post tonsillectomy morbidity. Pharmacol Pharmacother 3:254–258
Elhakim M, Ali NM, Rashed I, Riad MK, Refat M (2003) Dexamethasone reduces postoperative vomiting and pain after pediatric tonsillectomy. Can J Anesth 50:392–397
An K, Elkassabany NM, Liu J (2015) Dexamethasone as adjuvant to bupivacaine prolongs the duration of thermal antinociception and prevents bupivacaine-induced rebound hyperalgesia via regional mechanism in a mouse sciatic nerve block model. PLoS One 10:e0123459. https://doi.org/10.1371/journal.pone.0123459
Carr AS, Elliot D (2011) Otorhinolaryngology: anesthetic considerations. In: Bissonnette B (ed) Pediatric Anesthesia: Basic Principles, State of the Art, Future PMPH-USA, p 1707
Ferrari LR (2006) Adenotonsillectomy. In: Atlee JL (ed) Complications in Anesthesia, 2nd edn. Saunders Elsevier, Philadelphia, p 689
Acknowledgements
This study was carried out in Sisli Hamidiye Etfal Training and Research Hospital, Istanbul.
Funding
There are no financial conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kilinc, L., Türk, B., Türk, H.S. et al. Peritonsillar dexamethasone–bupivacaine vs. bupivacaine infiltration for post-tonsillectomy pain relief in children: a randomized, double-blind, controlled study. Eur Arch Otorhinolaryngol 276, 2081–2089 (2019). https://doi.org/10.1007/s00405-019-05472-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05472-y