Abstract
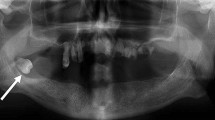
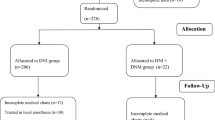
Possible airway compromise further complicates treatment of deep neck infections (DNI). Airway management is crucial, but factors affecting the method of choice are unclear. We retrospectively evaluated adult DNIs in a single tertiary center covering 10 years, with special attention on airway management. Patient data were retrieved from electronic data files from 2007 to 2016, and included adult patients with DNI operated through the neck. Of the 202 patients, 127 (63%) were male, with a median age of 47 years. Odontogenic (n = 74; 35%) infection was the most common etiology. Intubation was the most common method of airway management (n = 165; 82%), and most patients (n = 102; 50%) were extubated immediately after surgery. Tracheotomy was performed primarily for 35 (17%) patients, and secondarily for 25 (15%). Two patients were managed in local anesthesia. Altogether 80 (40%) patients required care in the intensive care unit for a median of 7 days. Median hospital stay was 6 days for intubated patients and 10 days for primarily tracheotomized (p = 0.036). DNI extended to the mediastinal space in 25 (12%) patients, most of whom with odontogenic infection (48%), and necrotizing fasciitis (32%). Odontogenic infection was the most common etiology for DNI with increased risk for mediastinal involvement. Intubation was most common type of airway management with high success in immediate extubation after surgery. The need for tracheotomy seemed to lead to a longer hospital care and was associated with a more severe clinical course.
Similar content being viewed by others
References
Wang LF, Kuo WR, Tsai SM, Huang KJ (2003) Characterizations of life-threatening deep cervical space infections: a review of one hundred ninety-six cases. Am J Otolaryngol 24:111–117
Boscolo-Rizzo P, Marchiori C, Montolli F, Vaglia A, Da Mosto MC (2006) Deep neck infections: a constant challenge. ORL J Otorhinolaryngol Relat Spec 68:259–265
Chi TH, Tsao YH, Yuan CH (2014) Influences of patient age on deep neck infection: clinical etiology and treatment outcome. Otolaryngol Head Neck Surg 151:586–590
Parhiscar A, Har-El G (2001) Deep neck abscess: a retrospective review of 210 cases. Ann Otol Rhinol Laryngol 110:1051–1054
Cho SY, Woo JH, Kim YJ et al (2016) Airway management in patients with deep neck infections: a retrospective analysis. Medicine (Baltimore) 95:e4125
Levitt GW (1970) Cervical fascia and deep neck infections. Laryngoscope 80:409–435
Karkos PD, Leong SC, Beer H, Apostolidou MT, Panarese A (2007) Challenging airways in deep neck space infections. Am J Otolaryngol 28:415–418
Piccirillo JF, Johnston A, Claybour P, Littenberg B, Creech C, Anderson S, Grove L, Costas I (2003) Comorbidity coding book. Washington University School of Medicine, St. Louis
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Barber BR, Dziegielewski PT, Biron VL, Ma A, Seikaly H (2014) Factors associated with severe deep neck space infections: targeting multiple fronts. J Otolaryngol Head Neck Surg 43:35
Kinzer S, Pfeiffer J, Becker S, Ridder GJ (2009) Severe deep neck space infections and mediastinitis of odontogenic origin: clinical relevance and implications for diagnosis and treatment. Acta Otolaryngol 129:62–70
Hidaka H, Yamaguchi T, Hasegawa J et al (2015) Clinical and bacteriological influence of diabetes mellitus on deep neck infection: systematic review and meta-analysis. Head Neck 37:1536–1546
Motahari SJ, Poormoosa R, Nikkhah M, Bahari M, Shirazy SM, Khavarinejad F (2015) Treatment and prognosis of deep neck infections. Indian J Otolaryngol Head Neck Surg 67:134–137
Kataria G, Saxena A, Bhagat S, Singh B, Kaur M, Kaur G (2015) Deep neck space infections: a study of 76 cases. Iran J Otorhinolaryngol 27:293–299
Candamourty R, Venkatachalam S, Babu MR, Kumar GS (2012) Ludwig’s Angina—an emergency: a case report with literature review. J Nat Sci Biol Med 3:206–208
Botha A, Jacobs F, Postma C (2015) Retrospective analysis of etiology and comorbid diseases associated with Ludwig’s Angina. Ann Maxillofac Surg 5:168–173
Cramer JD, Purkey MR, Smith SS, Schroeder JW Jr (2016) The impact of delayed surgical drainage of deep neck abscesses in adult and pediatric populations. Laryngoscope 126:1753–1760
Boscolo-Rizzo P, Stellin M, Muzzi E et al (2012) Deep neck infections: a study of 365 cases highlighting recommendations for management and treatment. Eur Arch Otorhinolaryngol 269:1241–1249
Potter JK, Herford AS, Ellis E (2002) Tracheotomy versus endotracheal intubation for airway management in deep neck space infections. J Oral Maxillofac Surg 60:349–354 (discussion 354–355)
Griffiths J, Barber VS, Morgan L, Young JD (2005) Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ 330:1243
Chen SJ, Ji N, Chen YX et al (2015) Management and maintenance of the airway in cervical necrotising fasciitis: a retrospective analysis of 15 cases. Br J Oral Maxillofac Surg 53:642–646
Blot F, Similowski T, Trouillet JL et al (2008) Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med 34:1779–1787
Mahafza T, Batarseh S, Bsoul N, Massad E, Qudaisat I, Al-Layla AE (2012) Early vs. late tracheostomy for the ICU patients: experience in a referral hospital. Saudi J Anaesth 6:152–154
Celakovsky P, Kalfert D, Tucek L et al (2014) Deep neck infections: risk factors for mediastinal extension. Eur Arch Otorhinolaryngol 271:1679–1683
Curtis JJ, Clark NC, McKenney CA et al (2001) Tracheostomy: a risk factor for mediastinitis after cardiac operation. Ann Thorac Surg 72:731–734
Pilarczyk K, Marggraf G, Dudasova M et al (2015) Tracheostomy after cardiac surgery with median sternotomy and risk of deep sternal wound infections: is it a matter of timing? J Cardiothorac Vasc Anesth 29:1573–1581
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author LT declares that she has no conflict of interest. Author LB declares that he has no conflict of interest. Author KA declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal participants performed by any of the authors. This research involved only patient charts. For this type of study formal consent is not required.
Funding
This study was supported by grants from the Sigrid Jusélius Foundation and the Finnish Otorhinolaryngology Research Foundation.
Rights and permissions
About this article
Cite this article
Tapiovaara, L., Bäck, L. & Aro, K. Comparison of intubation and tracheotomy in patients with deep neck infection. Eur Arch Otorhinolaryngol 274, 3767–3772 (2017). https://doi.org/10.1007/s00405-017-4694-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4694-5