Abstract
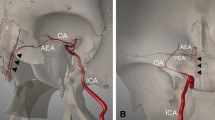
From 2006 to 2013, 12 patients with severe epistaxis refractory to prior conservative and surgical therapy were treated by superselective embolization of nasal arteries. Supersoft platinum microcoils with smallest diameters were used as the sole embolic agent in all cases. Coils were applied far distally in a stretched position for obtaining ideal target vessel superselectivity. The objective of this study is to evaluate efficacy and complications of superselective coil embolization for treatment of severe intractable epistaxis and to discuss results from an otorhinolaryngologic and an interventional neuroradiologic point of view. Retrospectively, all epistaxis inpatients between 2006 and 2013 were identified and subdivided by form of treatment: conservative, surgical and interventional therapy. Medical records of interventionally treated patients were reviewed for demographics, medical history, risk factors, clinical data, complications and short-term success, and patients were followed up for long-term success. Mean follow-up was 37 months. In 12 patients, 14 embolizations were carried out, with short-term success in 9 patients (75 %), while early post-interventional rebleeding occurred in 3 patients (25 %). Of 9 patients with short-term success, 1 died during stay, 1 was lost to follow-up and 1 had minor re-bleeding after 30 months. Six patients had short-term and long-term success. Before the first embolization, 3 ± 1 conservative and/or surgical procedures had been undertaken. Length of stay was 12.8 ± 3.6 days. 8 patients (67 %) received red cell concentrates. Most frequent complications were mucosal damage and nasal pain, but these were related to repeated packing and surgery. Typical embolic complications as neurological or visual impairment or soft tissue necrosis were not observed in any patient. From the otorhinolaryngologic point of view, surgery is the treatment of choice in severe refractory epistaxis, but in case of repeated failure, superselective microcoil embolization is a valuable addition to the therapeutic spectrum. From the interventional neuroradiologic point of view, superselective microcoil embolization is an effective, well tolerable and safe procedure and complications may be reduced in comparison to microparticle embolization. Modern supersoft microcoils with smallest diameters enable ideal superselectivity of the target vessels.


Similar content being viewed by others
References
Walker TW, Macfarlane TV, McGarry GW (2007) The epidemiology and chronobiology of epistaxis: an investigation of Scottish hospital admissions 1995–2004. Clin Otolaryngol 32(5):361–365. doi:10.1111/j.1749-4486.2007.01530.x
Melia L, McGarry GW (2011) Epistaxis: update on management. Curr Opin Otolaryngol Head Neck Surg 19(1):30–35. doi:10.1097/MOO.0b013e328341e1e9
Ando Y, Iimura J, Arai S, Arai C, Komori M, Tsuyumu M, Hama T, Shigeta Y, Hatano A, Moriyama H (2014) Risk factors for recurrent epistaxis: importance of initial treatment. Auris Nasus Larynx 41(1):41–45. doi:10.1016/j.anl.2013.05.004
Soyka MB, Nikolaou G, Rufibach K, Holzmann D (2011) On the effectiveness of treatment options in epistaxis: an analysis of 678 interventions. Rhinology 49(4):474–478. doi:10.4193/Rhino10.313
Cullen MM, Tami TA (1998) Comparison of internal maxillary artery ligation versus embolization for refractory posterior epistaxis. Otolaryngol Head Neck Surg 118(5):636–642. doi:10.1177/019459989811800512
Felippu A, Mora R, Guastini L (2011) Endoscopic transnasal cauterization of the anterior ethmoidal artery. Acta Otolaryngol 131(10):1074–1078. doi:10.3109/00016489.2011.593548
Metternich FU, Brusis T (1998) Ethmoid sinus operation for therapy of recurrence severe epistaxis. Laryngorhinootologie 77(10):582–586. doi:10.1055/s-2007-997030
Nouraei SA, Maani T, Hajioff D, Saleh HA, Mackay IS (2007) Outcome of endoscopic sphenopalatine artery occlusion for intractable epistaxis: a 10-year experience. The Laryngoscope 117(8):1452–1456. doi:10.1097/MLG.0b013e318065b86f
Willems PW, Farb RI, Agid R (2009) Endovascular treatment of epistaxis. AJNR Am J Neuroradiol 30(9):1637–1645. doi:10.3174/ajnr.A1607
Krajina A, Chrobok V (2014) Radiological diagnosis and management of epistaxis. Cardiovasc Intervent Radiol 37(1):26–36. doi:10.1007/s00270-013-0776-y
Gottumukkala R, Kadkhodayan Y, Moran CJ, Cross de WT 3rd, Derdeyn CP (2013) Impact of vessel choice on outcomes of polyvinyl alcohol embolization for intractable idiopathic epistaxis. J Vasc Interv Radiol 24(2):234–239. doi:10.1016/j.jvir.2012.10.001
Sadri M, Midwinter K, Ahmed A, Parker A (2006) Assessment of safety and efficacy of arterial embolisation in the management of intractable epistaxis. Eur Arch Otorhinolaryngol 263(6):560–566. doi:10.1007/s00405-006-0010-5
Andersen PJ, Kjeldsen AD, Nepper-Rasmussen J (2005) Selective embolization in the treatment of intractable epistaxis. Acta Oto-Laryngol 125(3):293–297. doi:10.1080/00016480410023029
Moreau S, De Rugy MG, Babin E, Courtheoux P, Valdazo A (1998) Supraselective embolization in intractable epistaxis: review of 45 cases. Laryngoscope 108(6):887–888. doi:10.1097/00005537-199806000-00018
Tseng EY, Narducci CA, Willing SJ, Sillers MJ (1998) Angiographic embolization for epistaxis: a review of 114 cases. Laryngoscope 108(4):615–619. doi:10.1097/00005537-199804000-00028
Elahi MM, Parnes LS, Fox AJ, Pelz DM, Lee DH (1995) Therapeutic embolization in the treatment of intractable epistaxis. Arch Otolaryngol Head Neck Surg 121(1):65–69
Elden L, Montanera W, Terbrugge K, Willinsky R, Lasjaunias P, Charles D (1994) Angiographic embolization for the treatment of epistaxis—a review of 108 cases. Otolaryngol Head Neck Surg 111(1):44–50
Vitek J (1991) Idiopathic intractable epistaxis: endovascular therapy. Radiology 181(1):113–116. doi:10.1148/radiology.181.1.1887018
Fukutsuji K, Nishiike S, Aihara T, Uno M, Harada T, Gyoten M, Imai S (2008) Superselective angiographic embolization for intractable epistaxis. Acta Oto-Laryngol 128(5):556–560. doi:10.1080/00016480701596070
Christensen NP, Smith DS, Barnwell SL, Wax MK (2005) Arterial embolization in the management of posterior epistaxis. Otolaryngol Head Neck Surg 133(5):748–753. doi:10.1016/j.otohns.2005.07.041
Leppanen M, Seppanen S, Laranne J, Kuoppala K (1999) Microcatheter embolization of intractable idiopathic epistaxis. Cardiovasc Intervent Radiol 22(6):499–503. doi:10.1007/S002709900439
Strach K, Schrock A, Wilhelm K, Greschus S, Tschampa H, Mohlenbruch M, Naehle CP, Jakob M, Gerstner AO, Bootz F, Schild HH, Urbach H (2011) Endovascular treatment of epistaxis: indications, management, and outcome. Cardiovasc Intervent Radiol 34(6):1190–1198. doi:10.1007/s00270-011-0155-5
Kramann B, Roth R, Schneider G, Uder M, Federspil P, Iro H (1998) Percutaneous transcatheter embolization in the treatment of refractory nontraumatic epistaxis. Hno 46(12):973–979. doi:10.1007/S001060050344
Oguni T, Korogi Y, Yasunaga T, Sadanaga T, Uozumi H, Kawanaka K, Sumi S, Takahashi M (2000) Superselective embolisation for intractable idiopathic epistaxis. Brit J Radiol 73(875):1148–1153
Cohen JE, Moscovici S, Gomori JM, Eliashar R, Weinberger J, Itshayek E (2012) Selective endovascular embolization for refractory idiopathic epistaxis is a safe and effective therapeutic option: technique, complications, and outcomes. J Clin Neurosci 19(5):687–690. doi:10.1016/j.jocn.2011.08.019
Duncan IC, Fourie PA, le Grange CE, van der Walt HA (2004) Endovascular treatment of intractable epistaxis–results of a 4-year local audit. S Afr Med J 94(5):373–378
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Seidel, D.U., Remmert, S., Brassel, F. et al. Superselective microcoil embolization in severe intractable epistaxis: an analysis of 12 consecutive cases from an otorhinolaryngologic and an interventional neuroradiologic point of view. Eur Arch Otorhinolaryngol 272, 3317–3326 (2015). https://doi.org/10.1007/s00405-014-3427-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3427-2