Abstract
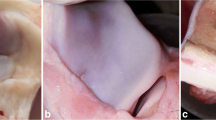
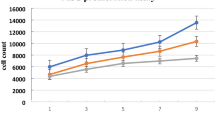
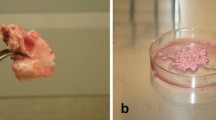
Although the regeneration process for injured cartilage requires an intact perichondrium, few studies have addressed the importance of the intact perichondrial layer in the regeneration of damaged cartilage. In this study, we evaluated the role of the perichondrium on regenerative activities in injured cartilage according to different degrees of perichondrial injury. Auricular cartilage harvested from six New Zealand white rabbits was irradiated with a 1,460-nm diode laser at two different power settings (0.3 or 0.5 W). Irradiated cartilage was reimplanted into a subperichondrial pocket under three different conditions: non-injured perichondrium (NPI), unilaterally injured perichondrium (UPI), or bilaterally injured perichondrium (BPI). Rabbits were sacrificed at 1, 2, and 4 weeks after reimplantation and the auricular cartilage was reharvested. A histopathological study using hematoxylin and eosin staining, a live/dead viability assay, and immunohistochemical staining for proliferating cell nuclear antigen were performed to evaluate structural changes and regenerative and proliferative activities of the injured chondrocytes. A modified array and restored boundary of chondrocytes were observed in the NPI and UPI groups. Regeneration of chondrocytes was prominent in the NPI and UPI groups, but was not observed in the BPI group. Proliferative activity of chondrocytes was observed only when the perichondrium was preserved in the NPI and UPI groups. In contrast, proliferative activity was not observed until 4 weeks in the BPI group. The degree of perichondrial injury affected proliferation and regeneration in injured elastic cartilage. In the case of unilateral perichondrial injury, the surgeon should be careful to avoid damaging the other side of the perichondrium, because at least a unilateral perichondrial layer is needed for the regeneration of elastic cartilage.





Similar content being viewed by others
References
Duynstee ML, Verwoerd-Verhoef HL, Verwoerd CD, Van Osch GJ (2002) The dual role of perichondrium in cartilage wound healing. Plast Reconstr Surg 110:1073–1079
ten Koppel PG, van Osch GJ, Verwoerd CD, Verwoerd-Verhoef HL (1998) Efficacy of perichondrium and a trabecular demineralized bone matrix for generating cartilage. Plast Reconstr Surg 102:2012–2020 (discussion 2021)
van Osch GJ, ten Koppel PG, van der Veen SW, Poppe P, Burger EH, Verwoerd-Verhoef HL (1999) The role of trabecular demineralized bone in combination with perichondrium in the generation of cartilage grafts. Biomaterials 20:233–240
Kim DW, Egan KK, O’Grady K, Toriumi DM (2005) Biomechanical strength of human nasal septal lining: comparison of the constituent layers. Laryngoscope 115:1451–1453
Muhammad IA, Nabil-ur R (2003) Complications of the surgery for deviated nasal septum. J Coll Physicians Surg Pak 13:565–568
Rettinger G, Kirsche H (2006) Complications in septoplasty. Facial Plast Surg 22:289–297
Karacalar A, Korkmaz A, Icten N (2005) A perichondrial flap for functional purposes in rhinoplasty. Aesthetic Plast Surg 29:256–260
Raunig H (2005) Antihelix plasty without modeling sutures. Arch Facial Plast Surg 7:334–341
Pountos I, Giannoudis PV (2005) Biology of mesenchymal stem cells. Injury 36(Suppl 3):S8–S12
Verwoerd-Verhoef HL, ten Koppel PG, van Osch GJ, Meeuwis CA, Verwoerd CD (1998) Wound healing of cartilage structures in the head and neck region. Int J Pediatr Otorhinolaryngol 43:241–251
Tcacencu I, Carlsoo B, Stierna P (2005) Cell origin in experimental repair of cricoid cartilage defects treated with recombinant human bone morphogenetic protein-2. Wound Repair Regen 13:341–349
Haberal Can I, Atilla P, Cakar AN, Onerci M (2008) An animal study on cartilage healing using auricular cartilage as a model. Eur Arch Otorhinolaryngol 265:307–311
Wong BJ, Chao KK, Kim HK, Chu EA, Dao X, Gaon M, Sun CH, Nelson JS (2001) The porcine and lagomorph septal cartilages: models for tissue engineering and morphologic cartilage research. Am J Rhinol 15:109–116
Rasouli A, Sun CH, Basu R, Wong BJ (2003) Quantitative assessment of chondrocyte viability after laser mediated reshaping: a novel application of flow cytometry. Lasers Surg Med 32:3–9
Lu Y, Hayashi K, Hecht P, Fanton GS, Thabit G 3rd, Cooley AJ, Edwards RB, Markel MD (2000) The effect of monopolar radiofrequency energy on partial-thickness defects of articular cartilage. Arthroscopy 16:527–536
Lu Y, Edwards RB 3rd, Kalscheur VL, Nho S, Cole BJ, Markel MD (2001) Effect of bipolar radiofrequency energy on human articular cartilage. Comparison of confocal laser microscopy and light microscopy. Arthroscopy 17:117–123
Zuger BJ, Ott B, Mainil-Varlet P, Schaffner T, Clemence JF, Weber HP, Frenz M (2001) Laser solder welding of articular cartilage: tensile strength and chondrocyte viability. Lasers Surg Med 28:427–434
Mainil-Varlet P, Monin D, Weiler C, Grogan S, Schaffner T, Zuger B, Frenz M (2001) Quantification of laser-induced cartilage injury by confocal microscopy in an ex vivo model. J Bone Joint Surg Am 83-A:566–571
Protsenko DE, Zemek A, Wong BJ (2008) Temperature dependent change in equilibrium elastic modulus after thermally induced stress relaxation in porcine septal cartilage. Lasers Surg Med 40:202–210
Gaon MD, Ho KH, Wong BJ (2003) Measurement of the elastic modulus of porcine septal cartilage specimens following Nd: YAG laser treatment. Lasers Med Sci 18:148–153
Helidonis E, Sobol E, Kavvalos G, Bizakis J, Christodoulou P, Velegrakis G, Segas J, Bagratashvili V (1993) Laser shaping of composite cartilage grafts. Am J Otolaryngol 14:410–412
Bruns J, Kersten P, Lierse W, Weiss A, Silbermann M (1994) The in vitro influence of different culture conditions on the potential of sheep rib perichondrium to form hyaline-like cartilage. Evaluation of gluing materials used for in vivo graft fixation. Virchows Arch 424:169–175
Eisemann ML (1983) The growth potential of autograft cartilage. An experimental study. Arch Otolaryngol 109:469–472
Bruns J, Meyer-Pannwitt U, Silbermann M (1992) The rib perichondrium. An anatomical study in sheep of a tissue used as transplant in the treatment of hyaline-cartilage defects. Acta Anat (Basel) 144:258–266
Acknowledgments
This research was supported by Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (MEST) (2012K1A4A3053142).
Conflict of interest
We have no actual or potential conflicts of interest in relation to this paper, nor do we have any financial relationship with the organization that sponsored this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ji-Hun Mo and Do-Joon Lee contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Mo, JH., Lee, DJ., Chung, PS. et al. Regenerative and proliferative activities of chondrocyte based on the degree of perichondrial injury in rabbit auricular cartilage. Eur Arch Otorhinolaryngol 271, 1573–1580 (2014). https://doi.org/10.1007/s00405-013-2769-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2769-5