Abstract
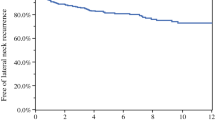
Despite an excellent prognosis, cervical lymph node (LN) metastases are common in patients with papillary thyroid cancer (PTC). The presence of metastasis is associated with an increased risk of locoregional recurrence, which significantly impairs quality of life and may decrease survival. Therefore, it has been an important determinant of the extent of lateral LN dissection in the initial treatment of PTC patients with lateral cervical metastasis. However, the optimal extent of therapeutic lateral neck dissection (ND) remains controversial. Optimizing the surgical extent of LN dissection is fundamental for balancing the surgical morbidity and oncological benefits of ND in PTC patients with lateral neck metastasis. We reviewed the currently available literature regarding the optimal extent of lateral LN dissection in PTC patients with lateral neck metastasis. Even in cases with suspicion of metastatic LN at the single lateral level or isolated metastatic lateral LN, the application of ND including all sublevels from IIa and IIb to Va and Vb may be overtreatment, due to the surgical morbidity. When there is no suspicion of LN metastasis at levels II and V, or when multilevel aggressive neck metastasis is not found, sublevel IIb and Va dissection may not be necessary in PTC patients with lateral neck metastasis. Thus consideration of the individualized optimal surgical extent of lateral ND is important when treating PTC patients with lateral cervical metastasis.

Similar content being viewed by others
References
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ et al (2009) Revised American Thyroid Association Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Siegel R, Ward E, Brawley O, Jemal A (2011) Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 61:212–236
Hundahl SA, Fleming ID, Fremgen AM, Menck HR (1998) A national cancer data base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995. Cancer 83:2638–2648
Gilliland FD, Hunt WC, Morris DM, Key CR (1997) Prognostic factors for thyroid carcinoma. A population-based study of 15,698 cases from the surveillance, epidemiology and end results (SEER) program 1973–1991. Cancer 79:564–573
Machens A, Hinze R, Thomusch O, Dralle H (2002) Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 26:22–28
Qubain SW, Nakano S, Baba M, Takao S, Aikou T (2002) Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery 131:249–256
Gimm O, Rath FW, Dralle H (1998) Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg 85:252–254
Machens A, Holzhausen HJ, Dralle H (2004) Skip metastases in thyroid cancer leaping the central lymph node compartment. Arch Surg 139:43–45
Chung YS, Kim JY, Bae JS, Song BJ, Kim JS, Jeon HM et al (2009) Lateral lymph node metastasis in papillary thyroid carcinoma: results of therapeutic lymph node dissection. Thyroid 19:241–246
Ferris R, Goldenberg D, Haymart MR, Shaha AR, Seth S, Sosa JA et al (2012) American Thyroid Association consensus review of the anatomy, terminology and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid [Epub ahead of print]
Farrag T, Lin F, Brownlee N, Kim M, Sheth S, Tufano RP (2009) Is routine dissection of level II-B and V-A necessary in patients with papillary thyroid cancer undergoing lateral neck dissection for FNA-confirmed metastases in other levels. World J Surg 33:1680–1683
Lim YC, Choi EC, Yoon YH, Koo BS (2010) Occult lymph node metastases in neck level V in papillary thyroid carcinoma. Surgery 147:241–245
Davidson HC, Park BJ, Johnson JT (2008) Papillary thyroid cancer: controversies in the management of neck metastasis. Laryngoscope 118:2161–2165
Kupferman ME, Weinstock YE, Santillan AA, Mishra A, Roberts D, Clayman GL et al (2008) Predictors of level V metastasis in well-differentiated thyroid cancer. Head Neck 30:1469–1474
Terrell JE, Welsh DE, Bradford CR, Chepeha DB, Esclamado RM, Hogikyan ND et al (2000) Pain, quality of life, and spinal accessory nerve status after neck dissection. Laryngoscope 110:620–626
Inoue H, Nibu K, Saito M, Otsuki N, Ishida H, Onitsuka T et al (2006) Quality of life after neck dissection. Arch Otolaryngol Head Neck Surg 132:662–666
Lee BJ, Wang SG, Lee JC, Son SM, Kim IJ, Kim YK (2007) Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 133:1028–1030
Lee J, Sung TY, Nam KH, Chung WY, Soh EY, Park CS (2008) Is level IIb lymph node dissection always necessary in N1b papillary thyroid carcinoma patients? World J Surg 32:716–721
Roh JL, Kim JM, Park CI (2008) Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Ann Surg Oncol 15:1177–1182
Koo BS, Yoon YH, Kim JM, Choi EC, Lim YC (2009) Predictive factors of level IIb lymph node metastasis in patients with papillary thyroid carcinoma. Ann Surg Oncol 16:1344–1347
Vayisoglu Y, Ozcan C, Turkmenoglu O, Gorur K, Unal M, Dag A et al (2010) Level IIb lymph node metastasis in thyroid papillary carcinoma. Eur Arch Otorhinolaryngol 267:1117–1121
King JM, Corbitt C, Miller FR (2011) Management of lateral cervical metastases in papillary thyroid cancer: patterns of lymph node distribution. Ear Nose Throat J 90:386–389
Pingpank JF Jr, Sasson AR, Hanlon AL, Friedman CD, Ridge JA (2002) Tumor above the spinal accessory nerve in papillary thyroid cancer that involves lateral neck nodes: a common occurrence. Arch Otolaryngol Head Neck Surg 128:1275–1278
Kim YS (2012) Patterns and predictive factors of lateral lymph node metastasis in papillary thyroid microcarcinoma. Otolaryngol Head Neck Surg 147:15–19
Yanir Y, Doweck I (2008) Regional metastases in well-differentiated thyroid carcinoma: pattern of spread. Laryngoscope 118:433–436
Kupferman ME, Patterson DM, Mandel SJ, LiVolsi V, Weber RS (2004) Safety of modified radical neck dissection for differentiated thyroid carcinoma. Laryngoscope 114:403–406
Caron NR, Tan YY, Ogilvie JB, Triponez F, Reiff ES, Kebebew E et al (2006) Selective modified radical neck dissection for papillary thyroid cancer-is level I, II and V dissection always necessary? World J Surg 30:833–840
Merdad M, Eskander A, Kroeker T, Freeman JL (2012) Predictors of level II and Vb neck disease in metastatic papillary thyroid cancer. Arch Otolaryngol Head Neck Surg 138:1030–1033
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MEST) (Grant number: 2012R1A1A2005393, 2013R1A2A2A01015281).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, JY., Koo, B.S. Individualized optimal surgical extent of the lateral neck in papillary thyroid cancer with lateral cervical metastasis. Eur Arch Otorhinolaryngol 271, 1355–1360 (2014). https://doi.org/10.1007/s00405-013-2630-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2630-x