Abstract
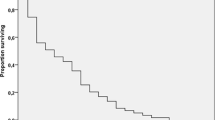
To study the role of surgery for symptom palliation in patients with advanced head and neck malignancy. Between 2000 and 2011, patients with locoregionally advanced cancer in the head and neck region, who chose surgical palliation for symptom control, were studied retrospectively. During the study period, 52 patients were included. The index tumour included carcinoma of the maxilla (23.1 %), tongue (19.2 %), larynx/hypopharynx (15.4 %), post-radiation sarcoma (11.5 %), primary sarcoma (11.5 %), carcinoma of the lower alveolus (11.5 %), nasal mucosal melanoma (3.9 %) and metastatic tumour in the head and neck region (3.9 %). The major symptoms included bleeding (53.9 %), tumour pain (19.2 %), dysphagia (11.5 %), non-healing ulcerations (7.7 %), airway obstruction (5.8 %) and pathological fracture of the mandible (1.9 %). Ligation of the carotid artery was performed in 10 patients, complete resection of tumour in 35, and surgical debulking of the tumour in 7 patients. Mean survival of the patients was 5.6 months. The majority of the patients achieved satisfactory and persistent control of symptoms. One patient died from pneumonia during the hospital stay, and the rest were discharged after a mean duration of 16.4 days. In selected patients, surgery is effective in palliating symptoms which are otherwise difficult to manage. Detailed planning and good communication is the key to success in improving the quality of dying.



Similar content being viewed by others
References
Hunter KD, Parkinson EK, Harrison PR (2005) Profiling early head and neck cancer. Nat Rev Cancer 5:127–135
Ellershaw J, Ward C (2003) Care of the dying patient: the last hours or days of life. BMJ 326:30–34
Coyle N, Adelhardt J, Foley KM, Portenoy RK (1990) Character of terminal illness in the advanced cancer patient: pain and other symptoms during the last four weeks of life. J Pain Symptom Manage 5:83–93
Good care of the dying patient—American Medical Association Council on Scientific Affairs. JAMA 1996; 275: 474–8
Lichter I, Hunt E (1990) The last 48 hours of life. J Pall Care 6:7–15
Steinhauser KE, Clipp E, McNeilly M, Christakis NA, McIntyre L, Tulsky JA (2000) In search of a good death: observations of patients, families and providers. Ann Intern Med 132:825–832
Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA (2000) Factors considered important at the end of life by patients, family, physicians and other care providers. JAMA 284:2476–2482
McCue JD (1995) The naturalness of dying. JAMA 273:1039–1043
Tobias JS (1944) Cancer of the head and neck. BMJ 038:961–966
SUPPORT Principal Investigators (1995) A controlled trail to improve care for seriously ill hospitalized patients. JAMA 274:1133–1138
Doyle D, Hanks GWC, MacDonald N (eds) (1998) Oxford book of palliative medicine, 2nd edn. Oxford University Press, Oxford
Cohen LM, Poppel DM, Cohn GM, Reiter GS (2001) A very good death: measuring quality of dying in end stage renal disease. J Palliat Med 4:167–172
Shedd DP, Carl A, Shedd C (1980) Problems of terminal head and neck cancer patients. Head Neck Surg 2(6):476–482
Bates MC, Shamsham FM (2003) Endovascular management of impending carotid rupture in a patient with advanced head and neck cancer. J Endovasc Ther 10(1):54–57
Broomfield SJ, Bruce IA, Luff DA, Birzgalis AR, Ashleigh RJ (2006) Endovascular management of the carotid blowout syndrome. J Laryngol Otol 120(8):694–697
Roh JL, Suh DC, Kim MR et al (2008) Endovascular management of carotid blowout syndrome in patients with head and neck cancers. Oral Oncol 44(9):844–850
Koutsimpelas D, Pitton M, Külkens C, Lippert BM, Mann WJ (2008) Endovascular carotid reconstruction in palliative head and neck cancer patients with threatened carotid blowout presents a beneficial supportive care measure. J Palliat Med 11(5):784–789
Townsend J, Frank AO, Fermont D et al (1990) Terminal cancer care and patients’ preference for place of death: a prospective study. BMJ 301:415–417
Higginson IJ (2003) Priorities and preferences for end of life care in England, Wales and Scotland.National Council for Hospice and Specialist Palliative Care Services. The Cicely Saunders Foundation, London
Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S (2003) Identifying potential indicators of the quality of end of life cancer care from administrative data. J Clin Oncol 21:1133–1138
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, J.Y.W., To, V.S.H., Wong, S.T.S. et al. Quality of dying in head and neck cancer patients: the role of surgical palliation. Eur Arch Otorhinolaryngol 270, 681–688 (2013). https://doi.org/10.1007/s00405-012-2059-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2059-7