Abstract
Purpose
Pregnancy-related psychophysiological changes are associated with the sleep alterations as the gestational weeks progress. The aim is to evaluate the effectiveness of sleep hygiene education programs during pregnancy.
Methods
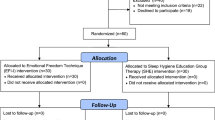
This prospective randomized controlled study based on pre–post-test after intervention consists of 30 studies and 30 control groups. Pregnant descriptive form, Beck Depression Index (BDI), Pittsburgh Sleep Quality Index (PSQI) and sleep hygiene index (SHI) questionnaires were used. Pregnant women with a score of 15 and above according to BDI were excluded from the study due to depression. Following the application of PSQI and SHI as a pretest, a sleep hygiene training program was applied to the intervention group twice with an interval of 15 days, and PSQI and SHI surveys were repeated as a posttest at the end of 1 month. End points with prespecified hypotheses were changes in sleep quality in different trimesters during antenatal follow-up (primary end point) and changes in sleep quality after the sleep hygiene education intervention from randomization to the end of the intervention period (secondary end point).
Results
90% of all pregnant women had poor sleep quality in the pre-test, and 93.3% in the post-test. In the intervention group, the pre-test PSQI score was 8.10 ± 1.80 and the post-test PSQI score was 8.37 ± 2.05 (p < 0.001). In the control group, the pre-test PSQI score was 8.23 ± 2.54 and the post-test PSQI score was 9.77 ± 2.54, and the worsening of sleep quality became more evident (p < 0.05). While the SHI in intervention group was 16.57 ± 5.64 in the pre-test, it was 10.30 ± 3.78 in the post-test after sleep hygiene training (p < 0.001). In the control group, the pre-test SHI scores increased from 14.50 ± 3.78 to the post-test scores of 16.60 ± 4.36, resulting in a decline in sleep hygiene and sleep quality (p < 0.05).
Conclusion
As the gestational week progressed, the deterioration in sleep quality increased. The poor sleep quality improved significantly after sleep hygiene education counseling. It is recommended to add sleep-related screenings to routine pregnancy follow-ups and to provide sleep hygiene education.



Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Sejbuk M, Mirończuk-Chodakowska I, Witkowska AM (2022) Sleep quality: A narrative review on nutrition, stimulants, and physical activity as ımportant factors. Nutrients. https://doi.org/10.3390/nu14091912
Peters AEJ, Verspeek LB, Nieuwenhuijze M, Harskamp-van Ginkel MW, Meertens RM (2023) The relation between sleep quality during pregnancy and health-related quality of life-a systematic review. J Matern Fetal Neonatal Med 36(1):2212829
Felder JN, Laraia B, Coleman-Phox K, Bush N, Suresh M, Thomas M, Adler N, Epel E, Prather AA (2018) Poor sleep quality, psychological distress, and the buffering effect of mindfulness training during pregnancy. Behav Sleep Med 16(6):611–624
Bacaro V, Benz F, Pappaccogli A, De Bartolo P, Johann AF, Palagini L et al (2020) Interventions for sleep problems during pregnancy: a systematic review. Sleep Med Rev 50:101234. https://doi.org/10.1016/j.smrv.2019.101234
Zafarghandi N, Hadavand S, Davati A, Mohseni SM, Kimiaiimoghadam F, Torkestani F (2012) The effects of sleep quality and duration in late pregnancy on labor and fetal outcome. J Matern Neonatal Med 25(5):535–537. https://doi.org/10.3109/14767058.2011.600370
Izci-Balserak B, Pien GW (2014) The relationship and potential mechanistic pathways between sleep disturbances and maternal hyperglycemia. Curr Diab Rep 14(2):459. https://doi.org/10.1007/s11892-013-0459-8
Dietrich SK, Francis-Jimenez CM, Knibbs MD, Umali IL, Truglio-Londrigan M (2016) Effectiveness of sleep education programs to improve sleep hygiene and/or sleep quality in college students: a systematic review. JBI Database Syst Rev Implement Rep 14(9):108–134
Yang Z, Zhu Z, Wang C, Zhang F, Zeng H (2022) Association between adverse perinatal outcomes and sleep disturbances during pregnancy: a systematic review and meta-analysis. J Matern Neonatal Med 35(1):166–174. https://doi.org/10.1080/14767058.2020.1711727
Sönmez A, Aksoy DY (2018) Effects of sleep hygiene training given to pregnant women with restless leg syndrome on their sleep quality. Sleep Breath 22(2):527–535. https://doi.org/10.1007/s11325-018-1619-5
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D et al (2015) Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep 38(6):843–844
Beck AT, Steer RA, Carbin MG (1988) Psychometric properties of the Beck depression inventory: twenty-five years of evaluaiton. Clin Psychol Rev 8(1):77–100
Hisli N (1989) Beck depresyon envanterinin üniversite öğrencileri için geçerliği güvenirliği. Psikoloji Dergisi. 7(3):13
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Ağargün MY, Kara HAÖ (1996) Pittsburg Uyku Kalitesi İndeksi’nin geçerliği ve güvenilirliği. Türk Psikiyatr Derg 7(107):15
Mastin DF, Bryson J, Corwyn R (2006) Assessment of sleep hygiene using the sleep hygiene index. J Behav Med 29(3):223–227
Ozdemir PG, Boysan M, Selvi Y, Yildirim A, Yilmaz E (2015) Psychometric properties of the Turkish version of the sleep hygiene index in clinical and nonclinical samples. Compr Psychiatry 59:135–140
Ko H, Shin J, Kim MY, Kim YH, Lee J, Kil KC et al (2012) Sleep disturbances in Korean pregnant and postpartum women. J Psychosom Obstet Gynecol 33(2):85–90
Yang Y, Mao J, Ye Z, Zeng X, Zhao H, Liu Y et al (2018) Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J Matern Neonatal Med 31(22):2980–2985
Rath TD, Baum KR, Kamstra BD, Schriever JA (2023) Integrating osteopathic manipulative treatment into prenatal care visits in a family medicine resident clinic. J Osteopath Med. https://doi.org/10.1515/jom-2023-0051
Bacaro V, Benz F, Pappaccogli A, De Bartolo P, Johann AF, Palagini L, Lombardo C, Feige B, Riemann D, Baglioni C (2020) Interventions for sleep problems during pregnancy: a systematic review. Sleep Med Rev 50:101234. https://doi.org/10.1016/j.smrv.2019.101234
Tsai S-Y, Lee C-N, Wu W-W, Landis CA (2016) Sleep hygiene and sleep quality of third-trimester pregnant women. Res Nurs Health 39(1):57–65
Ladyman C, Gander P, Huthwaite M, Sweeney B, Signal TL (2021) Sleep HAPi: a feasibility and descriptive analysis of an early and longitudinal sleep education ıntervention for pregnant women. Behav Sleep Med. https://doi.org/10.1080/15402002.2020.1772265
Liu Q, Song L, Fan G, Wu M, Bi J, Xu L, Xiong C, Xia W, Cao Z, Xu S, Wang Y (2023) Associations of self-reported sleep duration and sleep quality during pregnancy with newborn telomere length. Sleep Health 9(4):475–481. https://doi.org/10.1016/j.sleh.2023.03.001
Funding
The authors declare that no funds, grants or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NT, SAT and HA contributed to the study design and interpretation of the data. NT, SAT and AA contributed to the collection of data. SAT and HA contributed to the drafting and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conficts of interest to declare that are relevant to the content of this article.
Ethical approval
The study complied with the Declaration of Helsinki and was approved by the Gümüşhane University Scientific Research and Publication Ethics Committee, dated 14.04.2021 and numbered 2021/3.
Informed consent
Written informed consents were obtained from all participants before the recruitment to the study.
Ethical approval
The study complied with the Declaration of Helsinki and was approved by the Gümüşhane University Scientific Research and Publication Ethics Committee, dated 14.04.2021 and numbered 2021/3.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Turkmen, N., Alanya Tosun, S., Ayraler, A. et al. Sleep hygiene education program during pregnancy: a prospective randomized controlled study. Arch Gynecol Obstet (2024). https://doi.org/10.1007/s00404-024-07471-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-024-07471-9