Abstract
Purpose
What are the reproductive outcomes of women who had fertility preservation (FP) using either oocyte or embryo vitrification after fertility-sparing surgery (FSS) for a borderline ovarian tumor (BOT)?
Methods
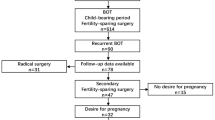
A retrospective, single-center cohort study was conducted between January 2013 and December 2021. Patients with BOT who resorted to FP by vitrifying oocytes or embryos were included. Both clinical and reproductive parameters were reviewed. The primary outcome was live birth.
Results
In total, thirteen patients who performed 31 FP cycles were included. Of those, six patients achieved eight live births after a mean follow-up period of 79 months. Three further pregnancies are still ongoing. All pregnancies/live births were obtained without using their cryopreserved oocytes or embryos.
Conclusion
Women who had FSS for BOT have favorable prospects of live offspring, even without the need to use their cryopreserved material. Fertility preservation in patients with BOT has to be considered as a tool to mitigate the risk of infertility that may arise in case of BOT recurrence requiring castrating surgery.

Similar content being viewed by others
References
Hart WR (2005) Borderline epithelial tumors of the ovary. Mod Pathol 18(Suppl 2):S33-50
Silverberg SG, Bell DA, Kurman RJ, Seidman JD, Prat J, Ronnett BM et al (2004) Borderline ovarian tumors: key points and workshop summary. Hum Pathol 35(8):910–917
Trope CG, Kaern J, Davidson B (2012) Borderline ovarian tumours. Best Pract Res Clin Obstet Gynaecol 26(3):325–336
Skirnisdottir I, Garmo H, Wilander E, Holmberg L (2008) Borderline ovarian tumors in Sweden 1960–2005: trends in incidence and age at diagnosis compared to ovarian cancer. Int J Cancer 123(8):1897–1901
Huang Y, Zhang W, Wang Y (2016) The feasibility of fertility-sparing surgery in treating advanced-stage borderline ovarian tumors: a meta-analysis. Taiwan J Obstet Gynecol 55(3):319–325
Morice P, Uzan C, Fauvet R, Gouy S, Duvillard P, Darai E (2012) Borderline ovarian tumour: pathological diagnostic dilemma and risk factors for invasive or lethal recurrence. Lancet Oncol 13(3):e103–e115
Gershenson DM, Sun CC, Bodurka D, Coleman RL, Lu KH, Sood AK et al (2009) Recurrent low-grade serous ovarian carcinoma is relatively chemoresistant. Gynecol Oncol 114(1):48–52
Longacre TA, McKenney JK, Tazelaar HD, Kempson RL, Hendrickson MR (2005) Ovarian serous tumors of low malignant potential (borderline tumors): outcome-based study of 276 patients with long-term (> or =5-year) follow-up. Am J Surg Pathol 29(6):707–723
Trope C, Davidson B, Paulsen T, Abeler VM, Kaern J (2009) Diagnosis and treatment of borderline ovarian neoplasms “the state of the art.” Eur J Gynaecol Oncol 30(5):471–482
Fauvet R, Demblocque E, Morice P, Querleu D, Darai E (2012) Behavior of serous borderline ovarian tumors with and without micropapillary patterns: results of a French multicenter study. Ann Surg Oncol 19(3):941–947
Darai E, Fauvet R, Uzan C, Gouy S, Duvillard P, Morice P (2013) Fertility and borderline ovarian tumor: a systematic review of conservative management, risk of recurrence and alternative options. Hum Reprod Update 19(2):151–166
du Bois A, Trillsch F, Mahner S, Heitz F, Harter P (2016) Management of borderline ovarian tumors. Ann Oncol 27(Suppl 1):i20–i22
Camatte S, Morice P, Pautier P, Atallah D, Duvillard P, Castaigne D (2002) Fertility results after conservative treatment of advanced stage serous borderline tumour of the ovary. BJOG 109(4):376–380
Gotlieb WH, Flikker S, Davidson B, Korach Y, Kopolovic J, Ben-Baruch G (1998) Borderline tumors of the ovary: fertility treatment, conservative management, and pregnancy outcome. Cancer 82(1):141–146
Gouy S, Maria S, Faron M, Maulard A, Pautier P, Leary A et al (2021) Results after conservative surgery of stage ii/iii serous borderline ovarian tumors. Ann Surg Oncol 28(7):3597–3604
Morris RT, Gershenson DM, Silva EG, Follen M, Morris M, Wharton JT (2000) Outcome and reproductive function after conservative surgery for borderline ovarian tumors. Obstet Gynecol 95(4):541–547
Fauvet R, Poncelet C, Boccara J, Descamps P, Fondrinier E, Darai E (2005) Fertility after conservative treatment for borderline ovarian tumors: a French multicenter study. Fertil Steril 83(2):284–290
De Munck N, Petrussa L, Verheyen G, Staessen C, Vandeskelde Y, Sterckx J et al (2015) Chromosomal meiotic segregation, embryonic developmental kinetics and DNA (hydroxy)methylation analysis consolidate the safety of human oocyte vitrification. Mol Hum Reprod 21(6):535–544
De Vos M, Smitz J, Thompson JG, Gilchrist RB (2016) The definition of IVM is clear-variations need defining. Hum Reprod 31(11):2411–2415
Delle Marchette M, Ceppi L, Andreano A, Bonazzi CM, Buda A, Grassi T et al (2019) Oncologic and fertility impact of surgical approach for borderline ovarian tumours treated with fertility sparing surgery. Eur J Cancer 111:61–68
Plett H, Harter P, Ataseven B, Heitz F, Prader S, Schneider S et al (2020) Fertility-sparing surgery and reproductive-outcomes in patients with borderline ovarian tumors. Gynecol Oncol 157(2):411–417
Poulain M, Vandame J, Tran C, Koutchinsky S, Pirtea P, Ayoubi JM (2020) Fertility preservation in borderline ovarian tumor patients and survivors. Horm Mol Biol Clin Investig 43(2):179–186
Peccatori FA, Azim HA Jr, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V et al (2013) Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24(Suppl 6):vi160–vi170
Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology (2013) Mature oocyte cryopreservation: a guideline. Fertil Steril 99(1):37–43
Porcu E, Venturoli S, Damiano G, Ciotti PM, Notarangelo L, Paradisi R et al (2008) Healthy twins delivered after oocyte cryopreservation and bilateral ovariectomy for ovarian cancer. Reprod Biomed Online 17(2):265–267
Khiat S, Provansal M, Bottin P, Saias-Magnan J, Metzler-Guillemain C, Courbiere B (2020) Fertility preservation after fertility-sparing surgery in women with borderline ovarian tumours. Eur J Obstet Gynecol Reprod Biol 253:65–70
Prasath EB, Chan ML, Wong WH, Lim CJ, Tharmalingam MD, Hendricks M et al (2014) First pregnancy and live birth resulting from cryopreserved embryos obtained from in vitro matured oocytes after oophorectomy in an ovarian cancer patient. Hum Reprod 29(2):276–278
Segers I, Mateizel I, Van Moer E, Smitz J, Tournaye H, Verheyen G et al (2015) In vitro maturation (IVM) of oocytes recovered from ovariectomy specimens in the laboratory: a promising “ex vivo” method of oocyte cryopreservation resulting in the first report of an ongoing pregnancy in Europe. J Assist Reprod Genet 32(8):1221–1231
Filippi F, Martinelli F, Somigliana E, Franchi D, Raspagliesi F, Chiappa V (2020) Oocyte cryopreservation in two women with borderline ovarian tumor recurrence. J Assist Reprod Genet 37(5):1213–1216
Huang JY, Buckett WM, Gilbert L, Tan SL, Chian RC (2007) Retrieval of immature oocytes followed by in vitro maturation and vitrification: a case report on a new strategy of fertility preservation in women with borderline ovarian malignancy. Gynecol Oncol 105(2):542–544
Segers I, Bardhi E, Mateizel I, Van Moer E, Schots R, Verheyen G et al (2020) Live births following fertility preservation using in-vitro maturation of ovarian tissue oocytes. Hum Reprod 35(9):2026–2036
Mulder RL, Font-Gonzalez A, Hudson MM, van Santen HM, Loeffen EAH, Burns KC et al (2021) Fertility preservation for female patients with childhood, adolescent, and young adult cancer: recommendations from the PanCareLIFE Consortium and the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol 22(2):e45–e56
Mangili G, Somigliana E, Giorgione V, Martinelli F, Filippi F, Petrella MC et al (2016) Fertility preservation in women with borderline ovarian tumours. Cancer Treat Rev 49:13–24
Masciangelo R, Bosisio C, Donnez J, Amorim CA, Dolmans MM (2018) Safety of ovarian tissue transplantation in patients with borderline ovarian tumors. Hum Reprod 33(2):212–219
Dolmans MM (2012) Safety of ovarian autotransplantation. Blood 120(22):4275–4276
Falcone F, Breda E, Ferrandina G, Malzoni M, Perrone AM, Cormio G et al (2021) Fertility-sparing treatment in advanced-stage serous borderline ovarian tumors. An analysis from the MITO14 study database. Gynecol Oncol 161(3):825–831
Jia SZ, Xiang Y, Yang JJ, Shi JH, Jia CW, Leng JH (2020) Oncofertility outcomes after fertility-sparing treatment of bilateral serous borderline ovarian tumors: results of a large retrospective study. Hum Reprod 35(2):328–339
Helpman L, Yaniv A, Beiner ME, Aviel-Ronen S, Perri T, Ben-Baruch G et al (2017) Fertility preservation in women with borderline ovarian tumors - how does it impact disease outcome? A cohort study. Acta Obstet Gynecol Scand 96(11):1300–1306
Acknowledgements
The authors would like to thank our study nurse E. Nulens for her continuous accessibility and administrative support.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
SC: Protocol and project development, data collection, analysis, and manuscript writing. EVM: Data collection and management. IDQ: Data collection and management. HT: Data analysis and manuscript editing. MDV: Protocol development, analysis, and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm not to have any potential conflicts of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki and was approved by the Ethical Committee of the Universitair Ziekenhuis Brussel (B.U.N. 1432021000518). The study was performed in accordance with the endorsed guidelines.
Human or animals rights
Not applicable.
Informed consent
Informed consent was obtained from all individual participants included in the study. At the moment of cryopreservation, the possibility of data-analysis for research was discussed and approved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cosyns, S., Van Moer, E., De Quick, I. et al. Reproductive outcomes in women opting for fertility preservation after fertility-sparing surgery for borderline ovarian tumors. Arch Gynecol Obstet 309, 2143–2152 (2024). https://doi.org/10.1007/s00404-024-07445-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07445-x