Abstract
Purpose
Our study aimed to determine the possible factors that might impact the probability of obtaining a euploid blastocyst following intracytoplasmic sperm injection (ICSI) and preimplantation genetic testing for aneuploidy (PGT-A) procedures in idiopathic recurrent pregnancy loss (RPL) patients.
Methods
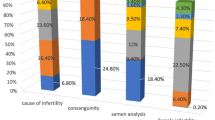
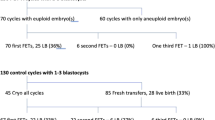
This single-center retrospective cohort analysis included 180 oocyte retrieval cycles of 166 women under 35 years old and those diagnosed with idiopathic RPL according to American Society of Reproductive Medicine (ASRM) guidelines. Trophectoderm biopsy and next-generation sequencing (NGS) were the techniques used. Patients were stratified by the number of previous losses (Group A: 2, Group B: 3, and Group C: > 3).
Results
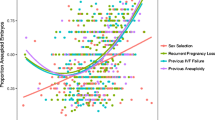
Baseline and embryological characteristics showed no statistically significant differences. The euploidy rate per analyzed blastocyst was comparable within the groups (63.3%, 58.2%, and 58.5%; p = 0.477). Logistic regression analyses confirmed that only the trophectoderm scores of A and B increased the probability of obtaining a euploid embryo [OR: 1.82, 95% CI (1.120–2.956), p: 0.016].
Conclusion
It is concluded that there was no correlation between the number of previous losses and the chance of finding at least one euploid embryo in ICSI cycles of women younger than 35 years.

Similar content being viewed by others
Data availability
Abbreviations
- AH:
-
Assisted hatching
- Array-CGH:
-
Array-based comparative genomic hybridization
- ASRM:
-
American Society of Reproductive Medicine
- BMI:
-
Body mass index
- E2 :
-
Estradiol
- GLMM:
-
Generalized linear mixed model
- hCG:
-
Human chorionic gonadotropin
- ICSI:
-
Intracytoplasmic sperm injection
- ICM:
-
Inner cell mass
- NGS:
-
Next-generation sequencing
- P4 :
-
Progesterone
- PGT-A:
-
Preimplantation genetic testing for aneuploidy
- POCs:
-
Products of conception
- RPL:
-
Recurrent pregnancy loss
- SART-CORS:
-
Society for assisted reproductive technology clinical outcomes reporting system
- SNP:
-
Single nucleotide polymorphism
- TV-USG:
-
Transvaginal ultrasound
References
Practice Committee of the American Society for Reproductive Medicine (2020) Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril 113(3):533–535. https://doi.org/10.1016/j.fertnstert.2019.11.025
Jaslow CR, Kutteh WH (2013) Effect of prior birth and miscarriage frequency on the prevalence of acquired and congenital uterine anomalies in women with recurrent miscarriage: a cross-sectional study. Fertil Steril 99(7):1916–1922. https://doi.org/10.1016/j.fertnstert.2013.01.152
Practice Committee of the American Society for Reproductive Medicine (2012) Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril 98(5):1103–1111. https://doi.org/10.1016/j.fertnstert.2012.06.048
Hassold TJ (1980) A cytogenetic study of repeated spontaneous abortions. Am J Hum Genet 32(5):723–730
Drugan A, Koppitch FC 3rd, Williams JC 3rd, Johnson MP, Moghissi KS, Evans MI (1990) Prenatal genetic diagnosis following recurrent early pregnancy loss. Obstet Gynecol 75(3 Pt 1):381–384
Stern JJ, Dorfmann AD, Gutierrez-Najar AJ, Cerrillo M, Coulam CB (1996) Frequency of abnormal karyotypes among abortuses from women with and without a history of recurrent spontaneous abortion. Fertil Steril 65(2):250–253. https://doi.org/10.1016/s0015-0282(16)58079-0
Daniely M, Aviram-Goldring A, Barkai G, Goldman B (1998) Detection of chromosomal aberration in fetuses arising from recurrent spontaneous abortion by comparative genomic hybridization. Hum Reprod 13(4):805–809. https://doi.org/10.1093/humrep/13.4.805
Nikitina TV, Sazhenova EA, Zhigalina DI, Tolmacheva EN, Sukhanova NN, Lebedev IN (2020) Karyotype evaluation of repeated abortions in primary and secondary recurrent pregnancy loss. J Assist Reprod Genet 37(3):517–525. https://doi.org/10.1007/s10815-020-01703-y
McCoy RC, Demko Z, Ryan A, Banjevic M, Hill M, Sigurjonsson S, Rabinowitz M, Fraser HB, Petrov DA (2015) Common variants spanning PLK4 are associated with mitotic-origin aneuploidy in human embryos. Hum Genet 348(6231):235–238. https://doi.org/10.1126/science.aaa3337
Stephenson MD, Awartani KA, Robinson WP (2002) Cytogenetic analysis of miscarriages from couples with recurrent miscarriage: a case-control study. Hum Reprod 17(2):446–451. https://doi.org/10.1093/humrep/17.2.446
Sullivan AE, Silver RM, LaCoursiere DY, Porter TF, Branch DW (2004) Recurrent fetal aneuploidy and recurrent miscarriage. Obstet Gynecol 104(4):784–788. https://doi.org/10.1097/01.AOG.0000137832.86727.e2
Wang Y, Cheng Q, Meng L, Luo C, Hu H, Zhang J, Cheng J, Xu T, Jiang T, Liang D et al (2017) Clinical application of SNP array analysis in first-trimester pregnancy loss: a prospective study. Clin Genet 91(6):849–858. https://doi.org/10.1111/cge.12926
Smits MAJ, van Maarle M, Hamer G, Mastenbroek S, Goddijn M, van Wely M (2020) Cytogenetic testing of pregnancy loss tissue: a meta-analysis. Reprod Biomed Online 40(6):867–879. https://doi.org/10.1016/j.rbmo.2020.02.001
Lee HL, McCulloh DH, Hodes-Wertz B, Adler A, McCaffrey C, Grifo JA (2015) In vitro fertilization with preimplantation genetic screening improves implantation and live birth in women age 40 through 43. J Assist Reprod Genet 32(3):435–444. https://doi.org/10.1007/s10815-014-0417-7
Chang J, Boulet SL, Jeng G, Flowers L, Kissin DM (2016) Outcomes of in vitro fertilization with preimplantation genetic diagnosis: an analysis of the United states assisted reproductive technology surveillance data, 2011–2012. Fertil Steril 105(2):394–400. https://doi.org/10.1016/j.fertnstert.2015.10.018
Bhatt SJ, Marchetto NM, Roy J, Morelli SS, McGovern PG (2021) Pregnancy outcomes following in vitro fertilization frozen embryo transfer (IVF-FET) with or without preimplantation genetic testing for aneuploidy (PGT-A) in women with recurrent pregnancy loss (RPL): a SART-CORS study. Hum Reprod 36(8):2339–2344. https://doi.org/10.1093/humrep/deab117
Chan C, Ryu M, Zwingerman R (2020) Preimplantation genetic testing for aneuploidy: A Canadian Fertility and Andrology Society Guideline. Reprod Biomed Online 42(1):105–116. https://doi.org/10.1016/j.rbmo.2020.10.020
Dahdouh EM (2021) Preimplantation genetic testing for aneuploidy: a review of the evidence. Obstet Gynecol 137(3):528–534. https://doi.org/10.1097/AOG.0000000000004295
Serdarogullari M, Coban O, Boynukalin FK, Bilgin EM, Findikli N, Bahceci M (2019) Successful application of a single warming protocol for embryos cryopreserved by either slow freezing or vitrification techniques. Syst Biol Reprod Med 65(1):12–19. https://doi.org/10.1080/19396368.2018.1487477
Gardner DK, Schoolcraft WB (1999) Culture and transfer of human blastocysts. Curr Opin Obstet Gynecol 11(3):307–311. https://doi.org/10.1097/00001703-199906000-00013
Zhao H, Tao W, Li M, Liu H, Wu K, Ma S (2019) Comparison of two protocols of blastocyst biopsy submitted to preimplantation genetic testing for aneuploidies: a randomized controlled trial. Arch Gynecol Obstet 299(5):1487–1493. https://doi.org/10.1007/s00404-019-05084-1
Wells D, Kaur K, Grifo J, Glassner M, Taylor JC, Fragouli E, Munne S (2014) Clinical utilization of a rapid low-pass whole genome sequencing technique for the diagnosis of aneuploidy in human embryos prior to implantation. J Med Genet 51(8):553–562. https://doi.org/10.1136/jmedgenet-2014-102497
Kung A, Munné S, Bankowski B, Coates A, Wells D (2015) Validation of next-generation sequencing for comprehensive chromosome screening of embryos. Reprod Biomed Online 31(6):760–769. https://doi.org/10.1016/j.rbmo.2015.09.002
Simón C, Rubio C, Vidal F, Gimenez C, Moreno C, Parrilla JJ, Pellicer A (1998) Increased chromosome abnormalities in human preimplantation embryos after in-vitro fertilization in patients with recurrent miscarriage. Reprod Fertil Dev 10(1):87–92. https://doi.org/10.1071/r98030
Pellicer A, Rubio C, Vidal F, Mínguez Y, Giménez C, Egozcue J, Remohí J, Simón C (1999) In vitro fertilization plus preimplantation genetic diagnosis in patients with recurrent miscarriage: an analysis of chromosome abnormalities in human preimplantation embryos. Fertil Steril 71(6):1033–1039. https://doi.org/10.1016/s0015-0282(99)00143-0
Rubio C, Simón C, Vidal F, Rodrigo L, Pehlivan T, Remohí J, Pellicer A (2003) Chromosomal abnormalities and embryo development in recurrent miscarriage couples. Hum Reprod 18(1):182–188. https://doi.org/10.1093/humrep/deg015
Platteau P, Staessen C, Michiels A, Van Steirteghem A, Liebaers I, Devroey P (2005) Preimplantation genetic diagnosis for aneuploidy screening in patients with unexplained recurrent miscarriages. Fertil Steril 83(2):393–397. https://doi.org/10.1016/j.fertnstert.2004.06.071
Rubio C, Buendía P, Rodrigo L, Mercader A, Mateu E, Peinado V, Delgado A, Milán M, Mir P, Simón C et al (2009) Prognostic factors for preimplantation genetic screening in repeated pregnancy loss. Reprod Biomed Online 18(5):687–693. https://doi.org/10.1016/s1472-6483(10)60015-6
Kort JD, McCoy RC, Demko Z, Lathi RB (2018) Are blastocyst aneuploidy rates different between fertile and infertile populations? J Assist Reprod Genet 35(3):403–408. https://doi.org/10.1007/s10815-017-1060-x
Liu XY, Fan Q, Wang J, Li R, Xu Y, Guo J, Wang YZ, Zeng YH, Ding CH, Cai B et al (2020) Higher chromosomal abnormality rate in blastocysts from young patients with idiopathic recurrent pregnancy loss. Fertil Steril 113(4):853–864. https://doi.org/10.1016/j.fertnstert.2019.11.016
Rubio C, Rodrigo L, Garcia-Pascual C, Peinado V, Campos-Galindo I, Garcia-Herrero S, Simón C (2019) Clinical application of embryo aneuploidy testing by next-generation sequencing. Biol Reprod 101(6):1083–1090. https://doi.org/10.1093/biolre/ioz019
Alfarawati S, Fragouli E, Colls P, Stevens J, Gutiérrez-Mateo C, Schoolcraft WB, Katz-Jaffe MG, Wells D (2011) The relationship between blastocyst morphology, chromosomal abnormality, and embryo gender. Fertil Steril 95(2):520–524. https://doi.org/10.1016/j.fertnstert.2010.04.003
Capalbo A, Rienzi L, Cimadomo D, Maggiulli R, Elliott T, Wright G, Nagy ZS, Ubaldi FM (2014) Correlation between standard blastocyst morphology, euploidy, and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod 29(6):1173–1181. https://doi.org/10.1093/humrep/deu033
Minasi MG, Colasante A, Riccio T, Ruberti A, Casciani V, Scarselli F, Spinella F, Fiorentino F, Varricchio MT, Greco E (2016) Correlation between aneuploidy, standard morphology evaluation and morphokinetic development in 1730 biopsied blastocysts: a consecutive case series study. Hum Reprod 31(10):2245–2254. https://doi.org/10.1093/humrep/dew183
Cimadomo D, Soscia D, Vaiarelli A, Maggiulli R, Capalbo A, Ubaldi FM, Rienzi L (2019) Looking past the appearance: a comprehensive description of the clinical contribution of poor-quality blastocysts to increase live birth rates during cycles with aneuploidy testing. Hum Reprod 34(7):1206–1214. https://doi.org/10.1093/humrep/dez078
Kutteh WH (2015) Novel strategies for the management of recurrent pregnancy loss. Semin Reprod Med 33(3):161–168. https://doi.org/10.1055/s-0035-1552586
van den Berg MM, van Maarle MC, van Wely M (1822) Goddijn M (2012) Genetics of early miscarriage. Biochim Biophys Acta 12:1951–1959. https://doi.org/10.1016/j.bbadis.2012.07.001
Wilson R, Geyer SH, Reissig L, Rose J, Szumska D, Hardman E, Prin F, McGuire C, Ramirez-Solis R, White J et al (2017) Highly variable penetrance of abnormal phenotypes in embryonic lethal knockout mice. Wellcome Open Res 27(1):1. https://doi.org/10.12688/wellcomeopenres.9899.2
Ewington LJ, Tewary S, Brosens JJ (2019) New insights into the mechanisms underlying recurrent pregnancy loss. J Obstet Gynaecol Res 45(2):258–265. https://doi.org/10.1111/jog.13837
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
TNE: protocol development, data analysis, manuscript writing. BFK: protocol development, manuscript writing. GM: data collection, data analysis. YZ: data analysis. AR: data collection. BM: manuscript editing. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was approved by the Institutional Review Board on 24 January 2019 with a reference number of 48.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Turgut, N.E., Boynukalin, F.K., Gultomruk, M. et al. The number of prior pregnancy losses does not impact euploidy rates in young patients with idiopathic recurrent pregnancy loss. Arch Gynecol Obstet 308, 1567–1575 (2023). https://doi.org/10.1007/s00404-023-07155-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07155-w