Abstract
Purpose
The number of elderly patients bothered by pelvic organ prolapse symptoms is growing rapidly. The aim of this study was to evaluate the relationship between age and surgical outcomes in women undergoing uterosacral ligament suspension for treatment of apical prolapse.
Methods
We performed a retrospective cohort study including women who underwent uterosacral ligament suspension between 2010 and 2020. The cohort was divided into two groups: (1) Patients 70 years or older; (2) Patients under the age of 70. Outcome measures included clinical, anatomical, and composite outcomes as well as patient satisfaction.
Results
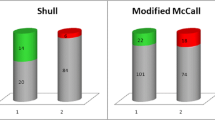
A total of 271 patients were included in the final analysis. Of them 209 patients were under age 70 and 62 patients 70 years or older. Mean age was 59 ± 6 vs. 73 ± 3 for the young and elderly age groups, respectively. Clinical success was high for both groups, reaching 94% vs. 89% for elderly and young patients, respectively (p = 0.34). Anatomical and composite outcome success were higher in the young age group (76% vs. 56%, p < 0.01 and 70% vs. 54%, p = 0.02, respectively); however, following multivariate analysis these differences were no longer statistically significant.
Following multivariate logistic regression analysis for the dependent parameter of anatomical success, increased pre-operative genital hiatus and vaginal surgical route were associated with anatomical failure while performing a concomitant posterior colporrhaphy increased likelihood for anatomical success.
Conclusion
Women over the age of 70 undergoing uterosacral ligament suspension for treatment of apical prolapse have comparable outcomes to younger patients.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, [HHC].
References
Barber MD, Maher C (2013) Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J 24(11):1783–1790
Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M (2017) Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet 389(10076):1323–1335
Ashcroft GS, Mills SJ, Ashworth JJ (2002) Ageing and wound healing. Biogerontology 3(6):337–345
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson FM (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123(6):1201–1206
Maher C, Feiner B, Baessler K et al (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014
Oh S, Shin EK, Hyun S, Jeon MJ (2021) Comparison of treatment outcomes for native tissue repair and sacrocolpopexy as apical suspension procedures at the time of hysterectomy for uterine prolapse. Sci Rep 11(1):3119
Kahn B, Varner RE, Murphy M et al (2022) Transvaginal mesh compared with native tissue repair for pelvic organ prolapse. Obstet Gynecol 139(6):975–985
Nager CW, Visco AG, Richter HE et al (2019) Effect of vaginal mesh hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: a randomized clinical trial. JAMA 322:1054–1065
Lipetskaia L, Gonzalez RR, Wu JM et al (2022) Thirty-six-month prospective study of transvaginal bovine graft vs native tissue repair for the treatment of pelvic organ prolapse. Urology 167:234–240
Schulten SF, Detollenaere RJ, IntHout J, Kluivers KB, Van Eijndhoven HW (2022) Risk factors for pelvic organ prolapse recurrence after sacrospinous hysteropexy or vaginal hysterectomy with uterosacral ligament suspension. Am J Obstet Gynecol 227(2):252.e1-252.e9
Cola A, Marino G, Milani R et al (2022) Native-tissue prolapse repair: Efficacy and adverse effects of uterosacral ligaments suspension at 10-year follow up. Int J Gynaecol Obstet 159(1):97–102
Shveiky D, Iglesia CB, Sarkar Das S et al (2020) Age-associated impairments in tissue strength and immune response in a rat vaginal injury model. Int Urogynecol J 31(7):1435–1441
Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL (2006) Effect of patient age on increasing morbidity and mortality following urogynecologic surgery. Am J Obstet Gynecol 194(5):1411–1417
Chapman GC, Sheyn D, Slopnick EA (2020) Perioperative safety of surgery for pelvic organ prolapse in elderly and frail patients. Obstet Gynecol 135(3):599–608
Sung VW, Joo K, Marques F, Myers DL (2009) Patient-reported outcomes after combined surgery for pelvic floor disorders in older compared to younger women. Am J Obstet Gynecol 201(5):534.e1–5
Joukhadar R, Radosa J, Paulus V et al (2019) Influence of patient’s age on the outcome of vaginal and laparoscopic procedures in urogynaecology. Geburtshilfe Frauenheilkd 79(9):949–958
Tinelli A, Malvasi A, Rahimi S et al (2010) Age-related pelvic floor modifications and prolapse risk factors in postmenopausal women. Menopause 17(1):204–212
Haj-Yahya R, Chill HH, Levin G, Reuveni-Salzman A, Shveiky D (2020) Laparoscopic uterosacral ligament hysteropexy vs total vaginal hysterectomy with uterosacral ligament suspension for anterior and apical prolapse: surgical outcome and patient satisfaction. J Minim Invasive Gynecol 27(1):88–93
Unger CA, Hickman LC, Mitchell-Handley B, Barber MD, Ridgeway B (2016) The incidence of perioperative adverse events in the very elderly undergoing urogynecologic surgery. Female Pelvic Med Reconstr Surg 22(6):425–429
Manodoro S, Frigerio M, Cola A, Spelzini F, Milani R (2018) Risk factors for recurrence after hysterectomy plus native-tissue repair as primary treatment for genital prolapse. Int Urogynecol J 29(1):145–151
Schulten SFM, Claas-Quax MJ, Weemhoff M et al (2022) Risk factors for primary pelvic organ prolapse and prolapse recurrence: an updated systematic review and meta-analysis. Am J Obstet Gynecol 227(2):192–208
Medina CA, Candiotti K, Takacs P (2008) Wide genital hiatus is a risk factor for recurrence following anterior vaginal repair. Int J Gynaecol Obstet 101(2):184–187
Vakili B, Zheng YT, Loesch H, Echols KT, Franco N, Chesson RR (2005) Levator contraction strength and genital hiatus as risk factors for recurrent pelvic organ prolapse. Am J Obstet Gynecol 192(5):1592–1598
Vaughan MH, Siddiqui NY, Newcomb LK et al (2018) Surgical alteration of genital hiatus size and anatomic failure after vaginal vault suspension. Obstet Gynecol 131(6):1137–1144
Jelovsek JE, Chagin K, Lukacz ES et al (2018) Models for predicting recurrence, complications, and health status in women after pelvic organ prolapse surgery. Obstet Gynecol 132(2):298–309
Sutkin G, Zyczynski HM, Sridhar A et al (2020) Association between adjuvant posterior repair and success of native tissue apical suspension. Am J Obstet Gynecol 222(2):161.e1-161.e8
Turner LC, Lavelle ES, Shepherd JP (2016) Comparison of complications and prolapse recurrence between laparoscopic and vaginal uterosacral ligament suspension for the treatment of vaginal prolapse. Int Urogynecol J 27(5):797–803
Diwan A, Rardin CR, Strohsnitter WC, Weld A, Rosenblatt P, Kohli N (2006) Laparoscopic uterosacral ligament uterine suspension compared with vaginal hysterectomy with vaginal vault suspension for uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 17(1):79–83
Huang L, Zhao Z, Wen J, Ling W, Miao Y, Wu J (2020) Cellular senescence: a pathogenic mechanism of pelvic organ prolapse (review). Mol Med Rep 22(3):2155–2162
Alperin M, Cook M, Tuttle LJ, Esparza MC, Lieber RL (2016) Impact of vaginal parity and aging on the architectural design of pelvic floor muscles. Am J Obstet Gynecol 215(3):312.e1–9
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Chill: project development, data collection, data analysis, manuscript writing and editing. Dick: project development, data collection, data analysis, manuscript writing and editing. Cohen: data collection, data analysis, manuscript editing. Ryvkin: manuscript writing and editing. Rosenbloom: data analysis, manuscript editing. Reuveni-Salzman: data collection, data analysis. Manuscript writing. Shveiky: project development, data analysis, manuscript writing and editing. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Hadassah Medical Center (IRB 0444-20-HMO).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chill, H.H., Dick, A., Cohen, A. et al. Surgical outcomes in patients aged 70 years and older following uterosacral ligament suspension: a comparative study. Arch Gynecol Obstet 307, 2033–2040 (2023). https://doi.org/10.1007/s00404-023-06974-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06974-1