Abstract
Introduction
There is no clear correlation between abnormal umbilical cord blood gas studies (UCGS) and adverse neonatal outcome in low-risk deliveries. We investigated the need for its routine use in low-risk deliveries.
Methods
We retrospectively compared maternal, neonatal, and obstetrical characteristics among low-risk deliveries (2014–2022) between “normal” and “abnormal” pH groups: A:normal pH ≥ 7.15; abnormal pH < 7.15; B: normal pH ≥ 7.15 and base excess (BE) > − 12 mmol/L; abnormal pH < 7.15 and BE ≤ We retrospectively compared 12 mmol/L; C: normal pH ≥ 7.1; abnormal pH < 7.1; D: normal pH > 7.1 and BE > − 12 mmol/L; abnormal pH < 7.1 and BE ≤ − 12 mmol/L.
Results
Of 14,338 deliveries, the rates of UCGS were: A—0.3% (n = 43); B—0.07% (n = 10); C—0.11% (n = 17); D—0.03% (n = 4).
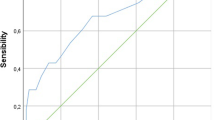
The primary outcome, composite adverse neonatal outcome (CANO) occurred in 178 neonates with normal UCGS (1.2%) and in only one case with UCGS (2.6%). The sensitivity and specificity of UCGS as a predictor of CANO were high (99.7–99.9%) and low (0.56–0.59%), respectively.
Conclusion
UCGS were an uncommon finding in low-risk deliveries and its association with CANO was not clinically relevant. Consequently, its routine use should be considered.

Similar content being viewed by others
References
Ahlberg M, Elvander C, Johansson S, Cnattingius S, Stephansson O (2017) A policy of routine umbilical cord blood gas analysis decreased missing samples from high-risk births. Acta Paediatr 106:43–48
Al Wattar BH, Honess E, Bunnewell S, Welton NJ, Quenby S, Khan KS, Zamora J, Thangaratinam S (2021) Effectiveness of intrapartum fetal surveillance to improve maternal and neonatal outcomes: a systematic review and network meta-analysis. CMAJ 193:E468-e477
Armstrong L, Stenson BJ (2007) Use of umbilical cord blood gas analysis in the assessment of the newborn. Arch Dis Child Fetal Neonatal Ed 92:F430-434
Fahey J, King TL (2005) Intrauterine asphyxia: clinical implications for providers of intrapartum care. J Midwifery Womens Health 50:498–506
Ferreira CS, Melo Â, Fachada AH, Solheiro H, Nogueira Martins N (2018) Umbilical cord blood gas analysis, obstetric performance and perinatal outcome. Rev Bras Ginecol Obstet 40:740–748
Goldaber KG, Gilstrap LC 3rd, Leveno KJ, Dax JS, McIntire DD (1991) Pathologic fetal acidemia. Obstet Gynecol 78:1103–1107
Gonen N, Gluck O, Zussman NM, Bar J, Kovo M, Weiner E (2019) The role of umbilical cord gas studies in the prediction of adverse neonatal outcomes in scheduled nonlaboring term singleton cesarean deliveries. Am J Obstet Gynecol MFM 1:119–127
Goodwin TM, Belai I, Hernandez P, Durand M, Paul RH (1992) Asphyxial complications in the term newborn with severe umbilical acidemia. Am J Obstet Gynecol 167:1506–1512
Herrera CA, Silver RM (2016) Perinatal asphyxia from the obstetric standpoint: diagnosis and interventions. Clin Perinatol 43:423–438
Johnson GJ, Salmanian B, Denning SG, Belfort MA, Sundgren NC, Clark SL (2021) Relationship Between Umbilical Cord Gas Values and Neonatal Outcomes: Implications for Electronic Fetal Heart Rate Monitoring. Obstet Gynecol 138:366–373
Kaasen A, Aanstad KJ, Pay ASD, Økland I, Blix E (2019) National survey of routines for intrapartum fetal monitoring in Norway. Acta Obstet Gynecol Scand 98:390–395
Kelly R, Ramaiah SM, Sheridan H, Cruickshank H, Rudnicka M, Kissack C, Becher JC, Stenson BJ (2018) Dose-dependent relationship between acidosis at birth and likelihood of death or cerebral palsy. Arch Dis Child Fetal Neonatal Ed 103:F567-f572
Khoury AD, Moretti ML, Barton JR, Shaver DC, Sibai BM (1991) Fetal blood sampling in patients undergoing elective cesarean section: a correlation with cord blood gas values obtained at delivery. Am J Obstet Gynecol 165:1026–1029
Leybovitz-Haleluya N, Wainstock T, Pariente G, Sheiner E (2021) Non-reassuring fetal heart rate patterns: Is it a risk factor for long- term pediatric cardiovascular diseases of the offspring? Early Hum Dev 155:105330
Low JA, Lindsay BG, Derrick EJ (1997) Threshold of metabolic acidosis associated with newborn complications. Am J Obstet Gynecol 177:1391–1394
Malin GL, Morris RK, Khan KS (2010) Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ 340:c1471
Martis R, Emilia O, Nurdiati DS, Brown J (2017) Intermittent auscultation (IA) of fetal heart rate in labour for fetal well-being. Cochrane Database Syst Rev 2:Cd008680
National Collaborating Centre for Ws, Children's H (2014) National Institute for Health and Care Excellence: Clinical Guidelines. Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. National Institute for Health and Care Excellence (UK) Copyright © 2014 National Collaborating Centre for Women's and Children's Health, London
Sabol BA, Caughey AB (2016) Acidemia in neonates with a 5-minute Apgar score of 7 or greater—what are the outcomes? Am J Obstet Gynecol 215:486.e481-486
Thoresen M (2015) Who should we cool after perinatal asphyxia? Semin Fetal Neonatal Med 20:66–71
Thorp JA, Dildy GA, Yeomans ER, Meyer BA, Parisi VM (1996) Umbilical cord blood gas analysis at delivery. Am J Obstet Gynecol 175:517–522
Vanspranghels R, Houfflin-Debarge V, Deken V, Rakza T, Maboudou P, Storme L, Ghesquiere L, Garabedian C (2020) Umbilical cord arterial and venous gases, ionogram, and glucose level for predicting neonatal morbidity at term. Eur J Obstet Gynecol Reprod Biol 252:181–186
Victory R, Penava D, Da Silva O, Natale R, Richardson B (2004) Umbilical cord pH and base excess values in relation to adverse outcome events for infants delivering at term. Am J Obstet Gynecol 191:2021–2028
White CR, Doherty DA, Henderson JJ, Kohan R, Newnham JP, Pennell CE (2010) Benefits of introducing universal umbilical cord blood gas and lactate analysis into an obstetric unit. Aust N Z J Obstet Gynaecol 50:318–328
Wiklund I, Ahlberg M, Dahlström A, Weichselbraun M, Sjörs G (2014) Routine testing of umbilical cord blood after normal delivery should be discontinued. Sex Reprod Healthc 5:165–166
Xodo S, Xodo L, Berghella V (2018) Delayed cord clamping and cord gas analysis at birth. Acta Obstet Gynecol Scand 97:7–12
Yeh P, Emary K, Impey L (2012) The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG 119:824–831
Zaigham M, Källén K, Olofsson P (2019) Gestational age-related reference values for Apgar score and umbilical cord arterial and venous pH in preterm and term newborns. Acta Obstet Gynecol Scand 98:1618–1623
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
EB: project development, data collection and management, data analysis, manuscript writing and editing. NG: project development, data collection and management, data analysis, manuscript writing and editing. IC: project development, data collection and management, data analysis, manuscript writing and editing. AS: project development. DJ: data collection. GB: project development. OG: data analysis. Eran Weiner: project development, data collection and management, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval number # 0215-20-WOMC dated 22.09.2020.
Consent to participate
This was a retrospective study; consent was not needed.
Consent to publish
There is no personal information in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonen, N., Cohen, I., Gluck, O. et al. Umbilical cord blood gases sampling in low-risk vaginal deliveries as a predictor of adverse neonatal outcome. Arch Gynecol Obstet 309, 523–531 (2024). https://doi.org/10.1007/s00404-023-06965-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06965-2