Abstract
Objective
Persistent high-risk human papillomavirus (hrHPV) infection is associated with most cervical cancers. This study aims to investigate the prevalence of and independent risk factors for hrHPV infection among women residing in rural areas of Shanxi Province, China.
Methods
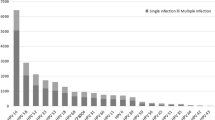
Data from the records of the cervical cancer screening programs for rural women in Shanxi Province were retrospectively collected. Women receiving primary HPV screening between January 2014 and December 2019 were included. The detection rate of hrHPV was calculated, and the independent risk factors for hrHPV infection were analyzed by multivariate logistic regression.
Results
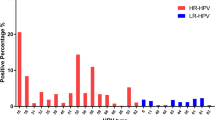
Among the women included, the overall infection rate of hrHPV was 14.01% (15,605/111,353), with the top five subtypes being HPV16 (24.79%), HPV52 (14.04%), HPV58 (10.26%), HPV18 (7.25%), and HPV53 (5.00%). The independent risk factors for hrHPV infection were specific geographical regions, testing years, older age, lower education level, inadequate previous screening, bacterial vaginosis, trichomonas vaginitis, and cervical polyps.
Conclusion
Rural women over 40 years of age, especially those who had never received screening, have a significantly increased risk for hrHPV infection and should be the target population with priority in cervical cancer screening.



Similar content being viewed by others
Date-sharing statement
The datasets generated during the current study are not publicly available yet, due to privacy concerns and ongoing additional research. Data can be made available for peer review on reasonable request through contacting the corresponding author.
Abbreviations
- HPV:
-
Human papillomavirus
- hrHPV:
-
High-risk human papillomavirus
- ACS:
-
American Cancer Society
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660. (Epub 2021/02/05. Cited in: Pubmed; PMID 33538338)
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66(2):115–132. https://doi.org/10.3322/caac.21338. (Epub 2016/01/26. Cited in: Pubmed; PMID 26808342)
Langsfeld E, Laimins LA (2016) Human papillomaviruses: research priorities for the next decade. Trends Cancer. 2(5):234–240. https://doi.org/10.1016/j.trecan.2016.04.001. (Epub 2016/09/13. Cited in: Pubmed; PMID 27617309)
Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V (2009) A review of human carcinogens—part B: biological agents. Lancet Oncol 10(4):321–322 (eng. Cited in: Pubmed; PMID 19350698)
Tota JE, Chevarie-Davis M, Richardson LA, Devries M, Franco EL (2011) Epidemiology and burden of HPV infection and related diseases: implications for prevention strategies. Prev Med 53(Suppl 1):S12-21. https://doi.org/10.1016/j.ypmed.2011.08.017. (Epub 2011/10/14. Cited in: Pubmed; PMID 21962466)
Sawaya GF, Smith-McCune K, Kuppermann M (2019) Cervical cancer screening: more choices in 2019. JAMA 321(20):2018–2019. https://doi.org/10.1001/jama.2019.4595. (eng. Cited in: Pubmed; PMID 31135834)
Chelimo C, Wouldes TA, Cameron LD, Elwood JM (2013) Risk factors for and prevention of human papillomaviruses (HPV), genital warts and cervical cancer. J Infect 66(3):207–217. https://doi.org/10.1016/j.jinf.2012.10.024. (Epub 2012/10/30. Cited in: Pubmed; PMID 23103285)
Li J, Huang R, Schmidt JE, Qiao YL (2013) Epidemiological features of Human Papillomavirus (HPV) infection among women living in Mainland China. Asian Pac J Cancer Prev 14(7):4015–4023. https://doi.org/10.7314/apjcp.2013.14.7.4015. (Epub 2013/09/03. Cited in: Pubmed; PMID 23991946)
Zahnd WE, Rodriguez C, Jenkins WD (2019) Rural-urban differences in human papillomavirus-associated cancer trends and rates. J Rural Health 35(2):208–215. https://doi.org/10.1111/jrh.12305. (Epub 2018/05/29. Cited in: Pubmed; PMID 29808500)
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1):12–19 (eng. Cited in: Pubmed; PMID 10451482)
Drolet M, Bénard É, Pérez N, Brisson M, Ali H, Boily M-C, Baldo V, Brassard P, Brotherton JML, Callander D, Checchi M, Chow EPF, Cocchio S, Dalianis T, Deeks SL, Dehlendorff C, Donovan B, Fairley CK, Flagg EW, Gargano JW, Garland SM, Grün N, Hansen BT, Harrison C, Herweijer E, Imburgia TM, Johnson AM, Kahn JA, Kavanagh K, Kjaer SK, Kliewer EV, Liu B, Machalek DA, Markowitz L, Mesher D, Munk C, Niccolai L, Nygård M, Ogilvie G, Oliphant J, Pollock KG, Purriños-Hermida MJ, Smith MA, Steben M, Söderlund-Strand A, Sonnenberg P, Sparen P, Tanton C, Wheeler CM, Woestenberg PJ, Yu BN (2019) Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. The Lancet 394(10197):497–509. https://doi.org/10.1016/s0140-6736(19)30298-3
Simms KT, Steinberg J, Caruana M, Smith MA, Lew J-B, Soerjomataram I, Castle PE, Bray F, Canfell K (2019) Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–99: a modelling study. Lancet Oncol 20(3):394–407. https://doi.org/10.1016/s1470-2045(18)30836-2
Fontham ETH, Wolf AMD, Church TR, Etzioni R, Flowers CR, Herzig A, Guerra CE, Oeffinger KC, Shih YT, Walter LC, Kim JJ, Andrews KS, DeSantis CE, Fedewa SA, Manassaram-Baptiste D, Saslow D, Wender RC, Smith RA (2020) Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin 70(5):321–346. https://doi.org/10.3322/caac.21628. (Epub 2020/07/31. Cited in: Pubmed; PMID 32729638)
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, Bray F (2020) Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health 8(2):e191–e203. https://doi.org/10.1016/s2214-109x(19)30482-6
Jiang L, Tian X, Peng D, Zhang L, Xie F, Bi C, Wang R, Wang J, Qi D (2019) HPV prevalence and genotype distribution among women in Shandong Province, China: Analysis of 94,489 HPV genotyping results from Shandong’s largest independent pathology laboratory. PLoS ONE 14(1):e0210311. https://doi.org/10.1371/journal.pone.0210311. (Epub 2019/01/18. Cited in: Pubmed; PMID 30653566)
Wang J, Tang D, Wang J, Zhang Z, Chen Y, Wang K, Zhang X, Ma C (2019) Genotype distribution and prevalence of human papillomavirus among women with cervical cytological abnormalities in Xinjiang. China. Hum Vaccin Immunother. 15(7–8):1889–1896. https://doi.org/10.1080/21645515.2019.1578598. (Epub 2019/02/09. Cited in: Pubmed; PMID 30735478)
Zhang C, Cheng W, Liu Q, Guan Q, Zhang Q (2019) Distribution of human papillomavirus infection: a population-based study of cervical samples from Jiangsu Province. Virol J. 16(1):67. https://doi.org/10.1186/s12985-019-1175-z. (Epub 2019/05/22. Cited in: Pubmed; PMID 31109361)
Teka B, Gizaw M, Ruddies F, Addissie A, Chanyalew Z, Skof AS, Thies S, Mihret A, Kantelhardt EJ, Kaufmann AM, Abebe T (2021) Population-based human papillomavirus infection and genotype distribution among women in rural areas of South Central Ethiopia. Int J Cancer 148(3):723–730. https://doi.org/10.1002/ijc.33278. (Epub 2020/09/03. Cited in: Pubmed; PMID 32875552)
Najioullah F, Dorival MJ, Joachim C, Dispagne C, Macni J, Abel S, Sulpicy C, Charpentier-Baltide H, Sainte-Rose D, Salomon-Frechou B, Dieye M, Veronique-Baudin J, Pre M, Marquet M, Wan-Ajouhu G, Janky E, Riethmuller D, Cesaire R, group Ds (2021) Genotype distribution of cervical HPV among Caribbean women in a population-based study in Martinique: the DEPIPAPUFR study. PLoS ONE 16(10):e0257915. https://doi.org/10.1371/journal.pone.0257915. (Epub 2021/10/08. Cited in: Pubmed; PMID 34618835)
Baloch Z, Yasmeen N, Li Y, Ma K, Wu X, Yang SH, Xia X (2017) Prevalence and risk factors for human papillomavirus infection among Chinese ethnic women in southern of Yunnan. China. Braz J Infect Dis. 21(3):325–332. https://doi.org/10.1016/j.bjid.2017.01.009. (Epub 2017/03/13. Cited in: Pubmed; PMID 28284657)
Amabebe E, Anumba D (2018) Lactobacilli the vaginal microenvironment: the physiologic role of. Front Med 5:181. https://doi.org/10.3389/fmed.2018.00181. (Cited In: Pubmed; PMID 29951482)
Torcia MG (2019) Interplay among vaginal microbiome, immune response and sexually transmitted viral infections. Int J Mol Sci. https://doi.org/10.3390/ijms20020266. (eng. Epub 2019/01/16. Cited in: Pubmed; PMID 30641869)
Temesgen MM, Alemu T, Shiferaw B, Legesse S, Zeru T, Haile M, Gelanew T (2021) Prevalence of oncogenic human papillomavirus (HPV 16/18) infection, cervical lesions and its associated factors among women aged 21–49 years in Amhara region, Northern Ethiopia. PLoS ONE 16(3):e0248949. https://doi.org/10.1371/journal.pone.0248949. (eng. Epub 2021/03/25. Cited in: Pubmed; PMID 33760866)
Yang J, Wang W, Wang Z, Wang Z, Wang Y, Wang J, Zhao W, Li D, Liu H, Hao M (2020) Prevalence, genotype distribution and risk factors of cervical HPV infection in Yangqu, China: a population-based survey of 10086 women. Hum Vaccin Immunother 16(7):1645–1652. https://doi.org/10.1080/21645515.2019.1689743. (Epub 2019/12/07. Cited in: Pubmed; PMID 31809222)
Chase D, Goulder A, Zenhausern F, Monk B, Herbst-Kralovetz M (2015) The vaginal and gastrointestinal microbiomes in gynecologic cancers: a review of applications in etiology, symptoms and treatment. Gynecol Oncol 138(1):190–200. https://doi.org/10.1016/j.ygyno.2015.04.036. (eng. Epub 2015/05/10. Cited in: Pubmed; PMID 25957158)
Kwasniewski W, Wolun-Cholewa M, Kotarski J, Warchol W, Kuzma D, Kwasniewska A, Gozdzicka-Jozefiak A (2018) Microbiota dysbiosis is associated with HPV-induced cervical carcinogenesis. Oncol Lett 16(6):7035–7047. https://doi.org/10.3892/ol.2018.9509. (Epub 2018/12/14. Cited in: Pubmed; PMID 30546437)
Barra F, Della Corte L, Noberasco G, Foreste V, Riemma G, Di Filippo C, Bifulco G, Orsi A, Icardi G, Ferrero S (2020) Advances in therapeutic vaccines for treating human papillomavirus-related cervical intraepithelial neoplasia. J Obstet Gynaecol Res 46(7):989–1006. https://doi.org/10.1111/jog.14276. (Epub 2020/05/12. Cited in: Pubmed; PMID 32390320)
Gardella B, Gritti A, Soleymaninejadian E, Pasquali MF, Riemma G, La Verde M, Schettino MT, Fortunato N, Torella M, Dominoni M (2022) New perspectives in therapeutic vaccines for HPV: a critical review. Medicina (Kaunas). https://doi.org/10.3390/medicina58070860. (Epub 2022/07/28. Cited in: Pubmed; PMID 35888579)
Acknowledgements
We thank the National Natural Science Foundation Commission of China for their generous support. We also thank all the data collectors, without whom this project would not have been possible.
Funding
This study was funded by the National Natural Science Foundation of China (82072891) and Shanxi Maternal and Child Health Hospital (2021009).
Author information
Authors and Affiliations
Contributions
RS and JC conceived and designed the study, having full access to all of the data in the study and taking responsibility for the content of the manuscript. RS and WJQ analyzed the data, took responsibility for the accuracy of the data analysis and wrote the first draft of the manuscript.ZHW and MZ reviewed the paper. RS, WJQ, JC, ZHW, and MZ contributed to the interpretation of the dataand clinical inputs. All authors were involved in the revision of themanuscript for important intellectual content and approved the final version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
This study was conducted with approval from the Ethics Committee of Shanxi Maternal and Child Health Hospital.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, R., Qi, W., Cai, J. et al. Independent risk factors for high-risk human papillomavirus infection among rural women in Shanxi Province, China: a population-based, case–control study. Arch Gynecol Obstet 308, 551–559 (2023). https://doi.org/10.1007/s00404-023-06959-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06959-0