Abstract
Purpose
To evaluate the effect of antenatal corticosteroid (ACS) treatment on neonatal outcomes in small for gestational age (SGA) infants born at 24–31 gestational weeks compared with non-SGA infants.
Methods
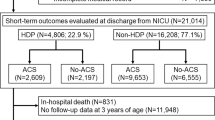
A population-based retrospective study was conducted that analyzed clinical data from the Neonatal Research Network of Japan database, which enrolls neonates born at < 32 gestational weeks and weighing 1500 g or less (n = 22,414). Propensity score matching (with the ratio of ACS to no-ACS groups of 1:1) was performed in SGA (n = 7028) and non-SGA (n = 15,386) infants, respectively. Univariate logistic and interaction analyses were performed to compare the short-term neonatal outcomes of infants with and without ACS treatment in utero.
Results
In the SGA and non-SGA infants, ACS treatment significantly reduced in-hospital mortality (odds ratio 0.67 95% confidence interval [0.50–0.88] and 0.62 [0.50–0.78], respectively), respiratory distress syndrome (0.77 [0.69–0.87] and 0.63 [0.58–0.68], respectively), and composite adverse outcomes (0.73 [0.58–0.91] and 0.57 [0.50–0.65], respectively). ACS treatment also significantly reduced intraventricular hemorrhage (grade III/IV), periventricular leukomalacia, and sepsis in the non-SGA infants, but not in the SGA infants. However, interaction analyses revealed no significant differences between the SGA and non-SGA infants in the efficacy of ACS treatment on short-term outcomes except for respiratory distress syndrome.
Conclusions
ACS treatment was associated with beneficial effects on mortality, respiratory distress syndrome, and adverse composite outcomes in extremely and very preterm SGA infants, with similar efficacy on all neonatal outcomes except for respiratory distress syndrome observed in the non-SGA infants.


Similar content being viewed by others
Availability of data and materials
Data that support the findings of this study are available from the corresponding author (TU) upon reasonable request and with permission from the Neonatal Research Network of Japan.
References
Madden JV, Flatley CJ, Kumar S (2018) Term small-for-gestational-age infants from low-risk women are at significantly greater risk of adverse neonatal outcomes. Am J Obstet Gynecol 218(5):525.e1-525.e9
Vollmer B, Edmonds CJ (2019) School age neurological and cognitive outcomes of fetal growth retardation or small for gestational age birth weight. Front Endocrinol 10:186
Crispi F, Miranda J, Gratacos E (2018) Long-term cardiovascular consequences of fetal growth restriction: biology, clinical implications, and opportunities for prevention of adult disease. Am J Obstet Gynecol 218(2s):S869-s879
Ray JG, Park AL, Fell DB (2017) Mortality in infants affected by preterm birth and severe small-for-gestational age birth weight. Pediatrics 140(6):e20171881
Paixao ES et al (2021) Risk of mortality for small newborns in Brazil, 2011–2018: a national birth cohort study of 17.6 million records from routine register-based linked data. Lancet Reg Health Americas 3:100045
Boghossian NS et al (2018) Morbidity and mortality in small for gestational age infants at 22 to 29 weeks’ gestation. Pediatrics 141(2):e20172533
Lee ACC et al (2013) National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health 1(1):e26–e36
Riskin-Mashiah S et al (2016) Antenatal corticosteroid treatment in singleton, small-for-gestational-age infants born at 24–31 weeks’ gestation: a population-based study. BJOG 123(11):1779–1786
Melamed N et al (2016) Antenatal corticosteroids and outcomes of small-for-gestational-age neonates. Obstet Gynecol 128(5):1001–1008
Ishikawa H et al (2015) The effects of antenatal corticosteroids on short- and long-term outcomes in small-for-gestational-age infants. Int J Med Sci 12(4):295–300
Marzouk A et al (2017) Prenatal and post-natal cost of small for gestational age infants: a national study. BMC Health Serv Res 17(1):221
Lee AC et al (2017) Estimates of burden and consequences of infants born small for gestational age in low and middle income countries with INTERGROWTH-21<sup>st</sup> standard: analysis of CHERG datasets. BMJ 358:j3677
McGoldrick E et al (2020) Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 12(12):CD004454
Amiya RM et al (2016) Antenatal corticosteroids for reducing adverse maternal and child outcomes in special populations of women at risk of imminent preterm birth: a systematic review and meta-analysis. PLoS ONE 11(2):e0147604
Magann EF et al (2017) Use of antenatal corticosteroids in special circumstances: a comprehensive review. Acta Obstet Gynecol Scand 96(4):395–409
Blankenship SA et al (2020) Antenatal corticosteroids in preterm small-for-gestational age infants: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 2(4):100215
Kumagai Y et al (2019) Contemporary challenges and developments: antenatal corticosteroid therapy. Curr Obstet Gynecology Rep 8(4):115–122
Kemp MW et al (2016) The clinical use of corticosteroids in pregnancy. Hum Reprod Update 22(2):240–259
Melamed N et al (2019) Neurodevelopmental disorders among term infants exposed to antenatal corticosteroids during pregnancy: a population-based study. BMJ Open 9(9):e031197
Sarid EB et al (2022) Neurological implications of antenatal corticosteroids on late preterm and term infants: a scoping review. Pediatr Res. https://doi.org/10.1038/s41390-022-02135-3
van der Merwe JL et al (2020) Long-term neuropathological and/or neurobehavioral effects of antenatal corticosteroid therapy in animal models: a systematic review. Pediatr Res 87(7):1157–1170
Astiz M et al (2020) The circadian phase of antenatal glucocorticoid treatment affects the risk of behavioral disorders. Nat Commun 11(1):3593
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46(3):399–424
Wada K (2017) Our challenges for the intact survival of newborn babies. Perinatology 28(1):1–3
Minakami H et al (2014) Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2014 edition. J Obstet Gynaecol Res 40(6):1469–1499
Ushida T et al (2020) Antenatal corticosteroids and outcomes in preterm twins. Obstet Gynecol 135(6):1387–1397
Itabashi K et al (2014) New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr Int 56(5):702–708
van Buuren S, Groothuis-Oudshoorn K (2011) mice: multivariate imputation by chained equations in R. J Stat Softw 45(3):1–67
Rubin DB. Multiple imputation for nonresponse in surveys. 2004.
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28(25):3083–3107
Farhad Pishgar NG (2021) Clémence Leyrat and Elizabeth Stuart, MatchThem: matching and weighting after multiple imputation. R J 13(2):292–305
Lumley T (2004) Analysis of complex survey samples. J Stat Softw 9(8):1–19
van Stralen G et al (2009) No short-term benefits of antenatal corticosteroid treatment in severely preterm growth restricted fetuses: a case-control study. Early Hum Dev 85(4):253–257
Kim WJ et al (2018) Antenatal corticosteroids and outcomes of preterm small-for-gestational-age neonates in a single medical center. Obstet Gynecol Sci 61(1):7–13
Morsi A, DeFranco D, Witchel SF (2018) The hypothalamic-pituitary-adrenal axis and the fetus. Horm Res Paediatr 89(5):380–387
Sheng JA et al (2021) The hypothalamic-pituitary-adrenal axis: development, programming actions of hormones, and maternal-fetal interactions. Front Behav Neurosci 14:601939
Goland RS et al (1993) Elevated levels of umbilical cord plasma corticotropin-releasing hormone in growth-retarded fetuses. J Clin Endocrinol Metab 77(5):1174–1179
Mericq V et al (2009) Differences in expression and activity of 11beta-hydroxysteroid dehydrogenase type 1 and 2 in human placentas of term pregnancies according to birth weight and gender. Eur J Endocrinol 161(3):419–425
Henley D et al (2016) Evidence for central hypercortisolism and elevated blood pressure in adolescent offspring of mothers with pre-eclampsia. Clin Endocrinol (Oxf) 85(4):583–589
Karrow NA (2006) Activation of the hypothalamic-pituitary-adrenal axis and autonomic nervous system during inflammation and altered programming of the neuroendocrine-immune axis during fetal and neonatal development: lessons learned from the model inflammagen, lipopolysaccharide. Brain Behav Immun 20(2):144–158
Gravett MG et al (2000) Intrauterine infection and preterm delivery: evidence for activation of the fetal hypothalamic-pituitary-adrenal axis. Am J Obstet Gynecol 182(6):1404–1413
Agresti A. Categorical data analysis, 3rd edition. 2012.
Gordijn SJ et al (2016) Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol 48(3):333–339
Finken MJJ et al (2018) Children born small for gestational age: differential diagnosis, molecular genetic evaluation, and implications. Endocr Rev 39(6):851–894
Acknowledgements
This study was supported by JSPS KAKENHI [grant number: JP 22H04923 (CoBiA)]. We would like to thank Editage for the English language editing.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Consortia
Contributions
TU, MN, and TK contributed to the concept and design of the study. TU, MN, and YK performed the statistical analyses. TU drafted the first version of this manuscript. TU, TK, NN, KF, YI, KI, YS, MH, and HK analyze and interpreted the data. TK and HK critically reviewed the manuscript, and all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Ethical approval
This study was approved by the Institutional Ethic Board of Nagoya University (approval number 2018-0026 on May 9, 2018), and the use of this database was permitted by the Japan Neonatal Network Executive Committee.
Consent to participate
Informed consent was obtained from parents at each facility.
Consent to publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
404_2022_6834_MOESM1_ESM.tif
Supplementary Figure 1. Flowchart of the cohort selection process for the additional analysis. The clinical data of infants born at <32 gestational weeks between 2008 and 2017 were obtained. A total of 22,671 infants were eligible for the multivariate logistic regression analysis (TIF 10515 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ushida, T., Nakatochi, M., Kobayashi, Y. et al. Antenatal corticosteroids and outcomes of small for gestational age infants born at 24–31 gestational weeks: a population-based propensity score matching analysis. Arch Gynecol Obstet 308, 1463–1471 (2023). https://doi.org/10.1007/s00404-022-06834-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06834-4