Abstract
Purpose
Intrapartum fetal death is devastating for both parents and medical caregivers. The purpose of this study was to evaluate the risk factors for intrapartum fetal death, which often influence management in subsequent pregnancies.
Methods
This population-based cohort study included all singleton deliveries between the years 1991–2016 at Soroka University Medical Center. Trends over the years, risk factors for intrapartum fetal death and the effect of day of the week were examined. A generalized estimation equation (GEE) model was used to control for confounders.
Results
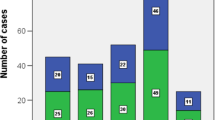
During the study period 344,536 deliveries were recorded, of which 251 (0.1%) suffered intrapartum fetal death. Rates did not change significantly over the years (p = 0.130, using the chi-square test for trends). Preterm delivery, placental abruption, uterine rupture, shoulder dystocia, congenital malformations, severe preeclampsia and fetal malpresentation were significantly more common in pregnancies complicated by intrapartum death. Using a GEE model; shoulder dystocia (aOR 23.8, 95% CI 9.9–57.3, p < 0.005), uterine rupture (aOR 19.0, 95% CI 7.0–51.4, p < 0.05), preterm delivery (aOR 11.9, 95% CI 8.6–16.5, p < 0.001), placental abruption (aOR 6.2, 95% CI 4.1–9.4, p < 0.001), fetal malpresentation (aOR 3.6, 95% CI 2.6–4.9, p < 0.005) and congenital malformations (aOR 2.6, 95% CI 1.9–3.5, p < 0.05) were all independent risk factors for intrapartum fetal death. Weekend deliveries were not at increased risk of intrapartum fetal death.
Conclusion
Several risk factors were identified for intrapartum fetal death, with shoulder dystocia demonstrating the highest risk. Unfortunately most factors are neither preventable nor predictable and interventions to decrease the rate of intrapartum fetal death remain elusive.
Similar content being viewed by others
References
De Bernis L, Kinney MV, Stones W, Ten Hoope-Bender P, Vivio D, Leisher SH et al (2016) Stillbirths: ending preventable deaths by 2030. Lancet 387(10019):703–716
Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I et al (2011) Stillbirths: where? When? Why? How to make the data count? Lancet 377(9775):1448–1463
Lawne JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hagan D, Flenady V et al (2016) Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 387(10018):587–603
Lawn J, Shibuya K, Stein C (2005) No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ 83:407–417
Barilovsky Y, Sheiner E, Wiznitzer A, Shahaf P, Levy A (2012) Risk factors for intrapartum fetal death and trends over the years. Arch Gynecol Obstet 285(2):323–329
Lawn JE, Yakoob M, Haws RA, Soomro T, Darmstadt GL, Bhutta ZA (2009) 3.2 million stillbirths: epidemiology and overview of the evidence review. BMC Pregnancy Childbirth 9(SUPPL. 1):1–17
Smith GC (2001) Life-table analysis of the risk of perinatal death at term and post term in singleton pregnancies. Am J Obstet Gynecol 184(3):489–496
Ohana O, Holcberg G, Sergienko R, Sheiner E (2011) Risk factors for intrauterine fetal death (1988–2009). J Matern Fetal Neonat Med 24(9):1079–1083
Estis-Deaton A, Sheiner E, Wainstock T, Landau D, Walfisch A (2017) The association between inadequate prenatal care and future healthcare use among offspring in the Bedouin population. Int J Gynecol Obstet 139:284–289
Abu-Ghanem S, Sheiner E, Sherf M, Wiznitzer A, Sergienko R, Shoham-Vardi I (2012) Lack of prenatal care in a traditional community: trends and perinatal outcomes. Arch Gynecol Obstet 285:1237–1242
Sheiner E, Shoham-Vardi I, Weitzman D, Gohar J, Carmi R (1998) Decisions regarding pregnancy termination among Bedouin couples referred to third level ultrasound clinic. Eur J Obstet Gynecol Reprod Biol 76(2):141–146
Spong CY, Iams J, Goldenberg R, Hauck FR, Willimger M (2011) Disparities in perinatal medicine: preterm birth, stillbirth and infant mortality. Obstet Gynecol 117(4):948–955
Fretts RC (2005) Etiology and prevention of still birth. Am J Obstet Gynecol 193(6):1923–1935
Althabe F, Moore JL, Gibbons L et al (2015) Adverse maternal and perinatal outcomes in adolescent pregnancies: the global network’s maternal newborn health registry study. Reprod Health 12:58
Liran D, Vardi IS, Sergienko R, Sheiner E (2013) Adverse perinatal outcome in teenage pregnancies: is it all due to lack of prenatal care and ethnicity? J Matern-Fetal Neonat Med 26(5):469–472
Salafia CM, Vogel CA, Vintzeleos AM, Bantham KF, Pezzulio J, Silberman L (1991) Placental pathologic findings in preterm birth. Am J Obstet Gynecol 165(4 Pt 1):934
Boghossian NS, Geraci M, Edwards EM, Horbar JD (2018) Morbidity and mortality in small for gestational age infants at 22 to 29 weeks gestation. Pediatrics 141(2):e20172533
Rsnik R (2002) Intrauterine growth restriction. Obstet Gynecol 99(3):490
Maoz O, Wainstock T, Sheiner E, Walfisch A (2019) Immediate perinatal outcomes of postterm deliveries. J Matern Fetal Neonat Med 32(11):1847–1852
Hedegaard M, Lidegaard O, Skovlund CW, Morch LS, Hedegaard M (2014) Reduction in stillbirths at term after new birth induction paradigm: results of a national intervention. BMJ Open 4:e005785
Ronel D, Wiznitzer A, Sergienko R, Zlotnik A, Sheiner E (2012) Trends, risk factors and pregnancy outcome in women with uterine rupture. Arch Gynecol Obstet 285(2):317–321. https://doi.org/10.1007/s00404-011-1977-8
Al-Zirqi I, Daltveit AK, Vangen S (2018) Infant outcome after complete uterine rupture. Am J Obstet Gynecol 219(1):109.e1-109.e8
Rackham O, Paize F, Weindling AM (2009) Cause of death in infants of women with pregestational diabetes mellitus and the relationship with glycemic control. Postgrad Med 121(4):26–32
Luo ZC, Liu S, Wilkins R, Kramer MS (2004) Fetal and infant health study group of the Canadian perinatal surveillance system risks of stillbirth and early neonatal death by day of week. CMAJ 170(3):337–341
Kleitman V, Feldman R, Walfisch A, Toledano R, Sheiner E (2016) Recurrent shoulder dystocia: is it predictable? Arch Gynecol Obstet 294(6):1161–1166. https://doi.org/10.1007/s00404-016-4139-1
Steiner N, Weintraub AY, Barski L, Sheiner E (2013) The unfavorable slope from mild preeclampsia through severe preeclampsia, to eclampsia. Pregnancy Hypertens 3(2):146–150
Palmer WL, Bottle A, Aylin P (2015) Association between day of delivery and obstetric outcomes: an observational study. BMJ 24(351):h5574
Hoyert DL, Gregory EC (2016) Cause of fetal death: data from the fetal death report 2014. Natl Vital Stat Rep 65(7):1
Funding
The authors declare that no funds, grants or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by EL, ES and GP. Data analysis was performed by TW. The first draft of the manuscript and all subsequent editions were written by SD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. LE: Data collection and management. DS: Manuscript writing/editing. SE: Protocol/project development. WT: Data analysis. PG: Protocol/project development.
Corresponding author
Ethics declarations
Conflict of interest
The authors conclude that they can report no conflicts of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee of Soroka University Medical Center (IRB 0358-19-SOR, 2019).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Davidesko, S., Levitas, E., Sheiner, E. et al. Critical analysis of risk factors for intrapartum fetal death. Arch Gynecol Obstet 308, 1239–1245 (2023). https://doi.org/10.1007/s00404-022-06811-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06811-x