Abstract
Purpose
The aim of the study was to estimate by a survival analysis model the hazard function (HF) for neonatal metabolic acidemia (MA) throughout the 2nd stage of labor (2STG) at the time of occurrence of a terminal bradycardia ≥ 10 min requiring expedited delivery, and the cumulative incidence function (CIF) for MA according with the duration of bradycardia stratified in 10–12 min and > 12 min.
Methods
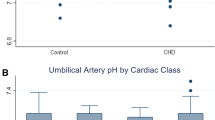
Singleton pregnancies experiencing terminal fetal bradycardia requiring expedited delivery in the 2STG at 38 + 0–41 + 3 weeks and delivering in the year 2019, were identified. The presence of MA (pH < 7 and/or BE ≤ − 12 mmol/L) was determined based on the acid–base status in the umbilical artery cord blood. Survival analysis was used to assess the hazard function (HF) and the cumulative incidence function (CIF) for MA occurring after terminal fetal bradycardia, at the 2STG.
Results
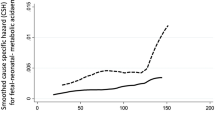
Out of a non-consecutive population of 12,331 pregnancies, there were 52 cases that fit the inclusion criteria. Twenty-four (46.2%) of those develop MA. Abnormal quantitative pH values and the HF for MA correlated with the duration of 2STG at the time of bradycardia onset, but not with bradycardia duration. After 60 min of duration of 2STG, the HF (or instantaneous rate of failure) increased dramatically (from 1.2 to 20 about at 120 min). At paired duration of 2STG, a higher CIF was observed for the terminal bradycardia > 12 min.
Conclusion
Forty-six percent of term fetuses with terminal bradycardia had MA at birth. Despite the low sensitivity and a non-significant association with quantitative pH values, the duration of terminal bradycardia in the 2STG is associated with a higher CIF for MA.



Similar content being viewed by others
Abbreviations
- FHR:
-
Fetal heart rate
- 2STG:
-
2nd stage of labor
- CTG:
-
Cardiotocography
- MA:
-
Metabolic acidemia
- CSH:
-
Cause-specific hazard
- CIF:
-
Cumulative incidence
- HR:
-
Hazard ratio
References
Turner JM, Mitchell MD, Kumar SS (2020) The physiology of intrapartum fetal compromise at term. Am J Obstet Gynecol 222(1):17–26
Graham EM, Ruis KA, Hartman AL, Northington FJ, Fox HE (2008) A systematic review of the role of intrapartum hypoxia ischemia in the causation of neonatal encephalopathy. Am J Obstet Gynecol 199(6):587–595
Block BS, Schlafer DH, Wentworth RA, Kreitzer LA, Nathanielsz PW (1990) Intrauterine asphyxia and the breakdown of physiologic circulatory compensation in fetal sheep. Am J Obstet Gynecol 162(5):1325–1331
Jensen A, Berger R (1991) Fetal circulatory responses to oxygen lack. J Dev Physiol 16(4):181–207
Pinas A, Chandraharan E (2016) Continuous cardiotocography during labour: analysis, classification and management. Best Pract Res Clin Obstet Gynaecol 30:33–47
Ugwumadu A (2013) Understanding cardiotocographic patterns associated with intrapartum fetal hypoxia and neurologic injury. Best Pract Res Clin Obstet Gynaecol 27(4):509–536
Ugwumadu A (2014) Are we (mis)guided by current guidelines on intrapartum fetal heart rate monitoring? Case for a more physiological approach to interpretation. BJOG 121(9):1063–1070
Piquard F, Hsiung R, Mettauer M, Schaefer A, Haberey P, Dellenbach P (1988) The validity of fetal heart rate monitoring during the second stage of labor. Obstet Gynecol 72:746–751
Sheiner E, Hadar A, Hallak M et al (2001) Clinical significance of fetal heart rate tracings during the second stage of labor. Obstet Gynecol 97:747–752
Weber T, Hahn-Pedersen S (1979) Normal values for fetal scalp tissue pH during labour. Br J Obstet Gynaecol 86:728–731
Tranquilli AL, Biagini A, Greco P, Di Tommaso M, Giannubilo SR (2013) The correlation between fetal bradycardia area in the second stage of labor and acidemia at birth. J Matern Fetal Neonatal Med 26:1425–1429
Cavoretto PI, Seidenari A, Amodeo S, Della Gatta AN, Nale R, Ismail YS, Candiani M, Farina A (2021) Quantification of posterior risk related to intrapartum FIGO 2015 criteria for cardiotocography in the second stage of labor. Fetal Diagn Ther 48(2):149–157
Freeman RK (2008) Medical and legal implications for necessary requirements to diagnose damaging hypoxic-ischemic encephalopathy leading to later cerebral palsy. Am J Obstet Gynecol 199(6):585–586
Hon EH (1958) The electronic evaluation of the fetal heart. Am J Obstet Gynecol 75:1215–1230
Beard RW, Filshie GM, Knight CA, Roberts GM (1971) The significance of the changes in the continuous fetal heart rate in the first stage of labour. J Obstet Gynaecol Br Commonw 78(10):865–881
Donker DK, van Geijn HP, Hasman A (1993) Interobserver variation in the assessment of fetal heart rate recordings. Eur J Obstet Gynecol Reprod Biol 52(1):21–28
Clark SL, Hankins GD (2003) Temporal and demographic trends in cerebral palsy–fact and fiction. Am J Obstet Gynecol 188(3):628–633
Ekengård F, Cardell M, Herbst A (2020) Low sensitivity of the new FIGO classification system for electronic fetal monitoring to identify fetal acidosis in the second stage of labor. Eur J Obstet Gynecol Reprod Biol X 9:100120
Ayres-de-Campos D, Spong CY, Chandraharan E (2015) FIGO intrapartum fetal monitoring expert consensus panel. FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int J Gynaecol Obstet 13:13–24
Santo S, Ayres-de-Campos D, Costa-Santos C, Schnettler W, Ugwumadu A, Da Graça LM (2017) Agreement and accuracy using the FIGO, ACOG and NICE cardiotocography interpretation guidelines. Acta Obstet Gynecol Scand 96(2):166–175
Ayres-de-Campos D, Arulkumaran S (2015) FIGO intrapartum fetal monitoring expert consensus panel. FIGO consensus guidelines on intrapartum fetal monitoring: physiology of fetal oxygenation and the main goals of intrapartum fetal monitoring. Int J Gynaecol Obstet 131(1):5–8
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Gimovsky AC, Berghella V (2016) Randomized controlled trial of prolonged second stage: extending the time limit vs usual guidelines. Am J Obstet Gynecol 214(361):e1-6
Siggaard-Andersen O (1971) An acid-base chart for arterial blood with normal and pathophysiological reference areas. Scand J Clin Lab Invest 27(3):239–245
Sabol BA, Caughey AB (2016) Acidemia in neonates with a 5-minute Apgar score of 7 or greater: what are the outcomes? Am J Obstet Gynecol 215(4):486–496
Low JA, Pickersgill H, Killen H, Derrick EJ (2001) The prediction and prevention of intrapartum fetal asphyxia in term pregnancies. Am J Obstet Gynecol 184:724–730
Di Tommaso M, Seravalli V, Cordisco A, Consorti G, Mecacci F, Rizzello F (2013) Comparison of five classification systems for interpreting electronic fetal monitoring in predicting neonatal status at birth. J Matern Fetal Neonatal Med 26:487–490
Elliot C, Warrick PA, Graham E, Hamilton EF (2010) Graded classification of fetal heart rate tracings: association with neonatal metabolic acidosis and neurologic morbidity. Am J Obstet Gynecol 202:258.e1-258.e8
Clark SL, Hamilton EF, Garite TJ, Timmins A, Warrick PA, Smith S (2017) The limits of electronic fetal heart rate monitoring in the prevention of neonatal metabolic acidemia. Am J Obstet Gynecol 216(2):163.e1-163.e6
Hasegawa J, Farina A, Turchi G, Hasegawa Y, Zanello M, Baroncini S (2013) Effects of epidural analgesia on labor length, instrumental delivery, and neonatal short-term outcome. J Anesth 27:43–47
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
AF: project development, conceptualization, methodology, software, validation, data analysis, supervision, resources, and manuscript writing (draft and revisions); PIC: conceptualization, methodology, manuscript writing (draft and revisions), visualization, and supervision; AS: data collection, visualization, and manuscript writing (draft and revisions); IFC: data collection and supervision; EI: supervision; CG: data collection, visualization, and writing (draft and revision); GG: data collection, visualization; GEC: data collection; DDDM: data collection; BM: resources and supervision; DM: conceptualization, resources, supervision; SA: data collection; LG: resources; MC: resources and supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This retrospective study was approved by the Local Ethics Committee of the Sant’Orsola Malpighi Hospital and conducted in agreement with ethical standards for human research established by the Declaration of Helsinki. The Ethics Committee code is DePreCar 805/2019.
Consent to participate
Informed consent was waived by Local Ethics Committee of the Sant’Orsola Malpighi Hospital due to retrospective nature of the study.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seidenari, A., Cavoretto, P.I., Carbone, I.F. et al. The cumulative incidence of neonatal metabolic acidemia after terminal bradycardia in the 2nd stage of labor: a survival-based model. Arch Gynecol Obstet 307, 1407–1414 (2023). https://doi.org/10.1007/s00404-022-06619-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06619-9