Abstract
Introduction and hypothesis
There is a complex relationship between obesity and pelvic organ prolapse. The objective of our study was to evaluate whether body mass index (BMI) changes the relationship between signs and symptoms of prolapse.
Methods
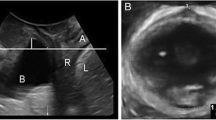
This was a retrospective observational study based on datasets of women seen in a tertiary urogynecological center with symptoms of pelvic floor and lower urinary tract dysfunction between April 2012 and October 2015. Patients underwent a structured interview, clinical examination (based on the POP-Q) and 4D transperineal ultrasound (TPUS). Offline assessment of sonographic organ descent was undertaken later, blinded to all patient data.
Results
Weight and BMI affect the relationship between symptoms and signs of prolapse. This effect is statistically highly significant. The more obese a patient is, the less likely she is to notice a given degree of objective prolapse, regardless of whether it is diagnosed clinically or on imaging.
Conclusions
In this retrospective study, we found a highly significant effect of weight and BMI on prolapse perception in the sense that obesity seems to mask prolapse while a low BMI increases the likelihood of a given degree of prolapse being noticed by the patient.
Similar content being viewed by others
Abbreviations
- POP:
-
Pelvic organ prolapse
- TPUS:
-
Trans perineal ultrasound
- BMI:
-
Body mass index
- POP-Q:
-
Pelvic organ prolapse quantification system
References
Giri A, Hartmann KE, Hellwege JN, Edwards DRV, Edwards TL (2017) Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol 217(1):11-26.e13
Young N, Atan IK, Rojas RG, Dietz HP (2018) Obesity: how much does it matter for female pelvic organ prolapse? Int Urogynecol J 29(8):1129–1134
Dietz H, Lekskulchai O (2007) Ultrasound assessment of pelvic organ prolapse: the relationship between prolapse severity and symptoms. Ultrasound Obstet Gynecol: Off J Int Soc Ultrasound Obstet Gynecol 29(6):688–691
Broekhuis SR, Fütterer JJ, Hendriks JC, Barentsz JO, Vierhout ME, Kluivers KB (2009) Symptoms of pelvic floor dysfunction are poorly correlated with findings on clinical examination and dynamic MR imaging of the pelvic floor. Int Urogynecol J 20(10):1169–1174
Whitcomb EL, Lukacz ES, Lawrence JM, Nager CW, Luber KM (2009) Prevalence and degree of bother from pelvic floor disorders in obese women. Int Urogynecol J 20(3):289
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Dietz HP (2010) Pelvic floor ultrasound: a review. Am J Obstet Gynecol 202(4):321–334
Dietz H, Mann K (2014) What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J 25(4):451–455
Dietz H, Haylen B, Broome J (2001) Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet Gynecol: Off J Int Soc Ultrasound Obstet Gynecol 18(5):511–514
Dietz HP (2019) Ultrasound in the assessment of pelvic organ prolapse. Best Pract Res Clin Obstet Gynaecol 54:12–30
Shek KL, Dietz HP (2015) What is abnormal uterine descent on translabial ultrasound? Int Urogynecol J 26(12):1783–1787
Ramalingam K, Monga A (2015) Obesity and pelvic floor dysfunction. Best Pract Res Clin Obstet Gynaecol 29(4):541–547
Kudish BI, Iglesia CB, Sokol RJ, Cochrane B, Richter HE, Larson J, Hendrix SL, Howard BV (2009) Effect of weight change on natural history of pelvic organ prolapse. Obstet Gynecol 113(1):81
de Oliveira MCE, de Lima VCdO, Pegado R, Silva-Filho EM, Fayh APT, Micussi MT (2019) Comparison of pelvic floor muscle training isolated and associated with weight loss: a randomized controlled trial. Arch Gynecol Obstet 300(5):1343–1351
Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, Wang W, Schaffer J (2005) Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 192(3):795–806
Whitcomb EL, Rortveit G, Brown JS, Creasman JM, Thom DH, Van Den Eeden SK, Subak LL (2009) Racial differences in pelvic organ prolapse. Obstet Gynecol 114(6):1271
Kudish BI, Iglesia CB, Gutman RE, Sokol AI, Rodgers AK, Gass M, O’Sullivan MJ, Larson J, Abu-Sitta M, Howard BV (2011) Risk factors for prolapse development in white, black, and Hispanic women. Female Pelvic Med Reconstr Surg 17(2):80
Shalom DF, Lin SN, St Louis S, Winkler HA (2012) Effect of age, body mass index, and parity on pelvic organ prolapse quantification system measurements in women with symptomatic pelvic organ prolapse. J Obstet Gynaecol Res 38(2):415–419
Subak L, Johnson C, Whitcomb E, Boban D, Saxton J, Brown J (2002) Does weight loss improve incontinence in moderately obese women? Int Urogynecol J 13(1):40–43
Young N, Atan IK, Rojas RG, Dietz HP (2015) Obesity: how much does it matter for female pelvic organ prolapse? Int Urogynecol J. https://doi.org/10.1007/s00192-017-3455-8
Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS (2005) Weight loss: a novel and effective treatment for urinary incontinence. J Urol 174(1):190–195
Lian W, Zheng Y, Huang H, Chen L, Cao B (2017) Effects of bariatric surgery on pelvic floor disorders in obese women: a meta-analysis. Arch Gynecol Obstet 296(2):181–189
Abdool Z, Dietz HP, Lindeque BG (2018) Interethnic variation in pelvic floor morphology in women with symptomatic pelvic organ prolapse. Int Urogynecol J 29(5):745–750
Cheung RY, Chan SS, Shek KL, Chung TK, Dietz HP (2019) Pelvic organ prolapse in Caucasian and East Asian women: a comparative study. Ultrasound Obstet Gynecol 53(4):541–545
Acknowledgements
The authors would like to thank A/Prof Clara shek and Dr Kristy Robledo for their help / advice with statistical analysis.
Funding
This study was unfunded.
Author information
Authors and Affiliations
Contributions
TF: Data acquisition, manuscript writing, data entry, data analysis, final approval. HPD: responsible for study conception and design, drafting the article and revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
HP Dietz has received lecture fees and travel support from GE Medical and Mindray. T Friedman has no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Friedman, T., Dietz, H.P. Does obesity change the perception of pelvic organ prolapse?. Arch Gynecol Obstet 305, 1491–1495 (2022). https://doi.org/10.1007/s00404-022-06430-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06430-6