Abstract
Purpose
To use machine learning and population data for testing the associations of preterm birth with socioeconomic status, gastroesophageal reflux disease (GERD) and medication history including proton pump inhibitors, sleeping pills and antidepressants.
Methods
Population-based retrospective cohort data came from Korea National Health Insurance Service claims data for all women who aged 25–40 years and gave births for the first time as singleton pregnancy during 2015–2017 (405,586 women). The dependent variable was preterm birth during 2015–2017 and 65 independent variables were included (demographic/socioeconomic determinants, disease information, medication history, obstetric information). Random forest variable importance (outcome measure) was used for identifying major determinants of preterm birth and testing its associations with socioeconomic status, GERD and medication history including proton pump inhibitors, sleeping pills and antidepressants.
Results
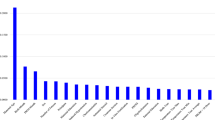
Based on random forest variable importance, major determinants of preterm birth during 2015–2017 were socioeconomic status (645.34), age (556.86), proton pump inhibitors (107.61), GERD for the years 2014, 2012 and 2013 (106.78, 105.87 and 104.96), sleeping pills (97.23), GERD for the years 2010, 2011 and 2009 (95.56, 94.84 and 93.81), and antidepressants (90.13).
Conclusion
Preterm birth has strong associations with low socioeconomic status, GERD and medication history such as proton pump inhibitors, sleeping pills and antidepressants. For preventing preterm birth, appropriate medication would be needed alongside preventive measures for GERD and the promotion of socioeconomic status for pregnant women.
Similar content being viewed by others
References
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R et al (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379:2162–2172
El-Serag HB, Sweet S, Winchester CC, Dent J (2014) Update on the epidemiology of gastrooesophageal reflux disease: a systematic review. Gut 63:871–880
Kim N, Lee SW, Cho SI, Park CG, Yang CH, Kim HS et al (2008) The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther 27:173–185
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol 89(Suppl 1):S159–S172
Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W (2014) Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res 93:1045–1053
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR et al (2019) Oral diseases: a global public health challenge. Lancet 394:249–260
Gilbert WM (2006) The cost of preterm birth: the low cost versus high value of tocolysis. BJOG 113(Suppl 3):4–9
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL et al (2019) Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 156:254-272.e11
Fill Malfertheiner S, Seelbach-Göbel B, Costa SD, Ernst W, Reuschel E, Zeman F et al (2017) Impact of gastroesophageal reflux disease symptoms on the quality of life in pregnant women: a prospective study. Eur J Gastroenterol Hepatol 29:892–896
Body C, Christie JA (2016) Gastrointestinal diseases in pregnancy: nausea, vomiting, hyperemesis gravidarum, gastroesophageal reflux disease, constipation, and diarrhea. Gastroenterol Clin North Am 45:267–283
Teshome A, Yitayeh A (2016) Relationship between periodontal disease and preterm low birth weight: systematic review. Pan Afr Med J 24:215
Manrique-Corredor EJ, Orozco-Beltran D, Lopez-Pineda A, Quesada JA, Gil-Guillen VF, Carratala-Munuera C (2019) Maternal periodontitis and preterm birth: systematic review and meta-analysis. Commun Dent Oral Epidemiol 47:243–251
Song JY, Kim HH, Cho EJ, Kim TY (2014) The relationship between gastroesophageal reflux disease and chronic periodontitis. Gut Liv 8:35–40
Boyapati R, Vudathaneni VKP, Nadella SB, Bollepalli AC, Marella Y, Adurty C (2020) Reflex gastroesophageal disorders and functional dyspepsia: potential confounding variables for the progression of chronic periodontitis: a clinical study. Int J Prev Med 11:138
Lee KS, Song IS, Kim ES, Ahn KH (2020) Determinants of spontaneous preterm labor and birth including gastroesophageal reflux disease and periodontitis. J Korean Med Sci 35:e105
Lee KS, Ahn KH (2020) Application of artificial intelligence in early diagnosis of spontaneous preterm labor and birth. Diagnostics (Basel) 10:733
Ouh YT, Lee KM, Ahn KH, Hong SC, Oh MJ, Kim HJ et al (2019) Predicting peripartum blood transfusion: focusing on pre-pregnancy characteristics. BMC Pregnancy Childb 19:477
Gill SK, O’Brien L, Einarson TR, Koren G (2009) The safety of proton pump inhibitors (PPIs) in pregnancy: a meta-analysis. Am J Gastroenterol 104:1541–1545
Li CM, Zhernakova A, Engstrand L, Wijmenga C, Brusselaers N (2020) Systematic review with meta-analysis: the risks of proton pump inhibitors during pregnancy. Aliment Pharmacol Ther 51:410–420
Jackson MA, Goodrich JK, Maxan ME, Freedberg DE, Abrams JA, Poole AC et al (2016) Proton pump inhibitors alter the composition of the gut microbiota. Gut 65:749–756
Eke AC, Saccone G, Berghella V (2016) Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG 123:1900–1907
Huybrechts KF, Sanghani RS, Avorn J, Urato AC (2014) Preterm birth and antidepressant medication use during pregnancy: a systematic review and meta-analysis. PLoS ONE 9:e92778
Källén B (2004) Neonate characteristics after maternal use of antidepressants in late pregnancy. Arch Pediatr Adolesc Med 158:312–316
Cantarutti A, Merlino L, Monzani E, Giaquinto C, Corrao G (2016) Is the risk of preterm birth and low birth weight affected by the use of antidepressant agents during pregnancy? A population-based investigation. PLoS ONE 11:e0168115
Montagnoli C, Zanconato G, Cinelli G, Tozzi AE, Bovo C, Bortolus R, Ruggeri S (2020) Maternal mental health and reproductive outcomes: a scoping review of the current literature. Arch Gynecol Obstet 302:801–819
Reichner CA (2015) Insomnia and sleep deficiency in pregnancy. Obstet Med 8:168–171
World Health Organization. Preterm birth. https://www.who.int/news-room/fact-sheets/detail/preterm-birth. Updated February 19, 2018. Accessed 1 Feb 2021
Campos-Berga L, Moreno-Giménez A, Vento M, Diago V, Hervás D, Sáenz P, Cháfer-Pericás C, García-Blanco A (2021) Cumulative life stressors and stress response to threatened preterm labour as birth date predictors. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-021-06251-z
Funding
This work was supported by the Korea University Medical Center (No. K1925051) and the Ministry of Science and ICT of South Korea under the Information Technology Research Center support program supervised by the IITP (Institute for Information & Communications Technology Planning & Evaluation) (No. IITP-2018-0-01405). The funder had no role in the design of the study, the collection, analysis and interpretation of the data and the writing of the manuscript.
The code and data presented in this study are not publicly available. But the code and data are available from the corresponding author upon reasonable request and under the permission of Korea National Health Insurance Service.
Author information
Authors and Affiliations
Contributions
KSL, ISS, ESK and KHA contributed to the design of the study. KSL, ISS, HIK and KHA contributed to the collection, analysis and interpretation of the data. KSL, ISS, ESK and KHA contributed to the writing and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interest to disclose.
Ethics approval and consent to participate
This retrospective cohort study was approved by the Institutional Review Board (IRB) of Korea University Anam Hospital on November 5, 2018 (2018AN0365). Informed consent was waived by the IRB.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, KS., Song, IS., Kim, E.S. et al. Association of preterm birth with medications: machine learning analysis using national health insurance data. Arch Gynecol Obstet 305, 1369–1376 (2022). https://doi.org/10.1007/s00404-022-06405-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06405-7