Abstract
Purpose
To compare oncological outcomes of laparoscopic radical hysterectomy (LRH) and abdominal radical hysterectomy (ARH) for low-risk cervical cancer.
Method
We retrospectively compared the 3-year overall survival (OS) and 3-year disease-free survival (DFS) of 1269 low-risk cervical cancer patients with FIGO 2009 stage IA2, IB1 and IIA1 with a tumour size < 2 cm, no lymphovascular space invasion (LVSI), superficial stromal invasion and no lymph node involvement on imaging, and who received LRH (n = 672) and ARH (n = 597) between 2009 and 2018 at 47 hospitals.
Results
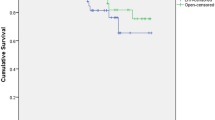
In the total study population, LRH and ARH showed similar 3-year OS (98.6% vs. 98.9%, P = 0.850) and DFS rates (95.7% vs. 96.4%, P = 0.285). LRH was not associated with worse 3-year OS (HR 0.897, 95% CI 0.287–2.808, P = 0.852) or DFS (HR 0.692, 95% CI 0.379–1.263, P = 0.230) as determined by multivariable analysis. After propensity score matching in 1269 patients, LRH (n = 551) and ARH (n = 551) still showed similar 3-year OS (98.4% vs. 98.8%, P = 0.704) and DFS rates (95.5% vs. 96.3%, P = 0.249). LRH was still not associated with worse 3-year OS (HR 0.816, 95% CI 0.262–2.541, P = 0.725) or DFS (HR 0.694, 95% CI 0.371–1.296, P = 0.251).
Conclusion
Among patients with low-risk cervical cancers < 2 cm, no LVSI, superficial stromal invasion, and no lymph node involvement on imaging, no significant differences were observed in 3-year OS or DFS rates between LRH and ARH.



Similar content being viewed by others
References
Koh W-J, Abu-Rustum NR, Bean S et al (2019) Cervical cancer, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 17:64–84. https://doi.org/10.6004/jnccn.2019.0001
Nezhat CR, Burrell MO, Nezhat FR et al (1992) Laparoscopic radical hysterectomy with paraaortic and pelvic node dissection. Am J Obstet Gynecol 166:864–865. https://doi.org/10.1016/0002-9378(92)91351-a
Malzoni M, Tinelli R, Cosentino F et al (2009) Total laparoscopic radical hysterectomy versus abdominal radical hysterectomy with lymphadenectomy in patients with early cervical cancer: our experience. Ann Surg Oncol 16:1316–1323. https://doi.org/10.1245/s10434-009-0342-7
Lee EJ, Kang H, Kim DH (2011) A comparative study of laparoscopic radical hysterectomy with radical abdominal hysterectomy for early-stage cervical cancer: a long-term follow-up study. Eur J Obstet Gynecol Reprod Biol 156:83–86. https://doi.org/10.1016/j.ejogrb.2010.12.016
Ditto A, Martinelli F, Bogani G et al (2015) Implementation of laparoscopic approach for type B radical hysterectomy: a comparison with open surgical operations. Eur J Surg Oncol 41:34–39. https://doi.org/10.1016/j.ejso.2014.10.058
Diver E, Hinchcliff E, Gockley A et al (2017) Minimally invasive radical hysterectomy for cervical cancer is associated with reduced morbidity and similar survival outcomes compared with laparotomy. J Minim Invasive Gynecol 24:402–406
Mendivil AA, Rettenmaier MA, Abaid LN et al (2016) Survival rate comparisons amongst cervical cancer patients treated with an open, robotic-assisted or laparoscopic radical hysterectomy: a five year experience. Surg Oncol 25:66–71
Guo J, Yang L, Cai J et al (2018) Laparoscopic procedure compared with open radical hysterectomy with pelvic lymphadenectomy in early cervical cancer: a retrospective study. Onco Targets Ther 11:5903–5908. https://doi.org/10.2147/OTT.S156064
Melamed A, Rauh-Hain JA, Ramirez PT (2019) Minimally invasive radical hysterectomy for cervical cancer: when adoption of a novel treatment precedes prospective, randomized evidence. J Clin Oncol 37:3069–3074. https://doi.org/10.1200/JCO.19.01164
Nam J-H, Park J-Y, Kim D-Y et al (2012) Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol 23:903–911. https://doi.org/10.1093/annonc/mdr360
Bogani G, Cromi A, Uccella S et al (2014) Laparoscopic versus open abdominal management of cervical cancer: long-term results from a propensity-matched analysis. J Minim Invasive Gynecol 21:857–862. https://doi.org/10.1016/j.jmig.2014.03.018
Sobiczewski P, Bidzinski M, Derlatka P et al (2009) Early cervical cancer managed by laparoscopy and conventional surgery comparison of treatment results. Int J Gynecol Cancer 19:1390–1395. https://doi.org/10.1111/IGC.0b013e3181ba5e88
Kim JHJW, Kim KK, Park SJ et al (2019) Comparative effectiveness of abdominal versus laparoscopic radical hysterectomy for cervical cancer in the postdissemination era. Cancer Res Treat 51:788–796. https://doi.org/10.4143/crt.2018.120
Uppal S, Rebecca Liu J, Kevin Reynolds R et al (2019) Trends and comparative effectiveness of inpatient radical hysterectomy for cervical cancer in the United States (2012–2015). Gynecol Oncol 152:133–138. https://doi.org/10.1016/j.ygyno.2018.09.027
dos Reis R, Andrade CEMC, Frumovitz M et al (2018) Radical hysterectomy and age: outcomes comparison based on a minimally invasive vs an open approach. J Minim Invasive Gynecol 25:1224–1230. https://doi.org/10.1016/j.jmig.2018.03.002
Yuan Z, Cao D, Yang JJ et al (2019) Laparoscopic vs. open abdominal radical hysterectomy for cervical cancer: a single-institution, propensity score matching study in China. Front Oncol 9:1107. https://doi.org/10.3389/fonc.2019.01107
Obermair A, Asher R, Pareja R et al (2020) Incidence of adverse events in minimally invasive vs open radical hysterectomy in early cervical cancer: results of a randomized controlled trial. Am J Obstet Gynecol 222:249.e1-249.e10
Ramirez PT, Frumovitz M, Pareja R et al (2018) Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 379:1895–1904. https://doi.org/10.1056/NEJMoa1806395
Melamed A, Margul DJ, Chen L et al (2018) Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med 379:1905–1914. https://doi.org/10.1056/NEJMoa1804923
Paik ES, Lim MC, Kim MH et al (2019) Comparison of laparoscopic and abdominal radical hysterectomy in early stage cervical cancer patients without adjuvant treatment: ancillary analysis of a korean gynecologic oncology group study (KGOG 1028). Gynecol Oncol 154:547–553. https://doi.org/10.1016/j.ygyno.2019.06.023
Kim SI, Cho JH, Seol A et al (2019) Comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1–IIA2 cervical cancer. Gynecol Oncol 153:3–12. https://doi.org/10.1016/j.ygyno.2019.01.008
Kim SI, Lee M, Lee S et al (2019) Impact of laparoscopic radical hysterectomy on survival outcome in patients with FIGO stage IB cervical cancer: a matching study of two institutional hospitals in Korea. Gynecol Oncol 155:75–82. https://doi.org/10.1016/j.ygyno.2019.07.019
Li Z, Chen C, Liu P, Duan H, Liu M, Xu Y, Li P, Zhang W, Jiang H, Bin X, Lang J (2021) Comparison of oncological outcomes and major complications between laparoscopic radical hysterectomy and abdominal radical hysterectomy for stage IB1 cervical cancer with a tumour size less than 2 cm. Eur J Surg Oncol 47(8):2125–2133. https://doi.org/10.1016/j.ejso.2021.03.238
Zhang X-R, Li Z-Q, Sun L-X, Liu P, Li Z-H, Li P-F, Zhao H-W, Chen B-L, Ji M, Wang L, Kang S, Lang J-H, Mao C, Chen C-L (2021) Cohort profile: Chinese cervical cancer clinical study. Front Oncol 11:690275. https://doi.org/10.3389/fonc.2021.690275
Li W, Liu P, Zhao W et al (2020) Effects of preoperative radiotherapy or chemoradiotherapy on postoperative pathological outcome of cervical cancer—from the large database of 46,313 cases of cervical cancer in China. Eur J Surg Oncol 46:148–154. https://doi.org/10.1016/j.ejso.2019.09.188
Chen B, Ji M, Li P et al (2020) Comparison between robot-assisted radical hysterectomy and abdominal radical hysterectomy for cervical cancer: a multicentre retrospective study. Gynecol Oncol. https://doi.org/10.1016/j.ygyno.2020.02.019
Chen C, Wang W, Liu P et al (2019) Survival after abdominal Q-M type B versus C2 radical hysterectomy for early-stage cervical cancer. Cancer Manag Res 11:10909–10919. https://doi.org/10.2147/CMAR.S220212
Liang C, Liu P, Cui Z et al (2020) Effect of laparoscopic versus abdominal radical hysterectomy on major surgical complications in women with stage IA-IIB cervical cancer in China, 2004–2015. Gynecol Oncol 156:115–123. https://doi.org/10.1016/j.ygyno.2019.10.032
Kong T-W, Chang S-J, Piao X et al (2016) Patterns of recurrence and survival after abdominal versus laparoscopic/robotic radical hysterectomy in patients with early cervical cancer. J Obstet Gynaecol Res 42:77–86. https://doi.org/10.1111/jog.12840
Lin F, Pan L, Li L et al (2014) Effects of a simulated CO2 pneumoperitoneum environment on the proliferation, apoptosis, and metastasis of cervical cancer cells in vitro. Med Sci Monit 20:2497–2503. https://doi.org/10.12659/MSM.891179
Selman TJ, Mann C, Zamora J et al (2008) Diagnostic accuracy of tests for lymph node status in primary cervical cancer: a systematic review and meta-analysis. CMAJ 178:855–862. https://doi.org/10.1503/cmaj.071124
Acknowledgements
We thank Min Hao (The Second Hospital of ShanXi Medical University), Bin Ling (China-Japan Friendship Hospital), Lixin Sun and Hongwei Zhao (Shanxi Cancer Hospital), Jihong Liu and Lizhi Liang (Sun Yat-sen University Cancer Center), Lihong Lin and Yu Guo (Anyang Tumor Hospital), Li Wang (The Affiliated Tumor Hospital of Zhengzhou University), Weidong Zhao (Anhui Provincial Cancer Hospital), Yan Ni (The Yuncheng Central Hospital of Shanxi Province), Wentong Liang and Donglin Li (Guizhou Provincial People`s Hospital), Xuemei Zhan and Mingwei Li (Jiangmen Central Hospital), Weifeng Zhang (Ningbo Women & Children’s Hospital), Peiyan Du (The Affiliated Cancer Hospital and Institute of Guangzhou Medical University), Ziyu Fang (Liuzhou Workers’ Hospital), Rui Yang (Shenzhen Hospital of Peking University), Long Chen (Qingdao Municipal Hospital), Encheng Dai and Ruilei Liu (Linyi People’s Hospital), Yuanli He and Mubiao Liu (Zhujiang Hospital, Southern Medical University), Jilong Yao and Zhihua Liu (Shenzhen Maternity & Child Health Hospital), Xueqin Wang (The Fifth Affiliated Hospital of Southern Medical University), Anwei Lu (Maternal and Child Health Hospital of Guiyang Province), Shuangling Jin (Peace Hospital affiliated to Changzhi Medical College), Ben Ma (Guangzhou First People’s Hospital), Zhonghai Wang (Shenzhen Nanshan People’s Hospital), Lin Zhu (The Second Hospital of Shandong University), Hongxin Pan (The Third Affiliated Hospital of Shenzhen University), Qianyong Zhu (No. 153. Center Hospital of Liberation Army/Hospital No. 988 of the Chinese People’s Liberation Army Joint Support Force), Dingyuan Zeng and Zhong Lin (Maternal and Child Health Care Hospital of Liuzhou), Xiaohong Wang (Laiwu People’s Hospital/Jinan City People’s Hospital), and Bin Zhu (The Affiliated Yiwu Women and Children Hospital of Hangzhou Medical College) for their contribution during the data collection.
Funding
This study received funding from the National Science and Technology Support Program of China (2014BAI05B03), the National Natural Science Fund of Guangdong (2015A030311024), and the Science and Technology Plan of Guangzhou (158100075).
Author information
Authors and Affiliations
Contributions
All authors approved the final version of the study. ZL, CC, PL and AL contributed equally to the work. ZL: data management, manuscript writing, data analysis. CC: project development, data management, data analysis. PL: project development, manuscript editing. AL: data collection, manuscript editing. HZ: data collection, figure production. XZ: data collection, figure production. HD: data collection, table production. PL: data collection, table production. WZ: data collection, validation. JY: data collection, validation. DL: data collection, validation. HJ: data collection, interpretation. ML: data collection, interpretation. XB: data analysis. JL: project development, data management.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical approval
This study has been approved by the Ethics Committee of Nanfang Hospital affiliated with Southern Medical University (Guangzhou, China) (ethical number: NFEC-2017–135, clinical research registration number: CHiCTR1800017778; International Clinical Trials Registry Platform Search Port, http://apps.who.int/trialsearch/). The ethical committee decided that no consent for participation was necessary, because the study was retrospective.
Informed consent
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Z., Chen, C., Liu, P. et al. Comparison between laparoscopic and abdominal radical hysterectomy for low-risk cervical cancer: a multicentre retrospective study. Arch Gynecol Obstet 305, 449–458 (2022). https://doi.org/10.1007/s00404-021-06185-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06185-6