Abstract
Purpose
Knowledge of adolescent and adult phenotypes of women with polycystic ovary syndrome (PCOS) might drive opportune management. The aim of this study was to compare metabolic and obesity biomarkers between adolescent and adult women with PCOS.
Methods
This observational study compared biomarkers of obesity and metabolism derangements between adolescent (n = 62) and adult (n = 248) women with PCOS. Predictors of metabolic syndrome (MS) were investigated using univariate and multivariate binary logistic regression analysis.
Results
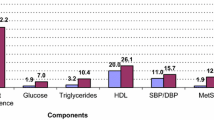
The postmenarcheal age of adolescents was 4.9 ± 0.03 years. Systolic blood pressure was lower in adolescents than in adults (112.3 mmHg vs 117.0 mmHg, p = 0.001) Diastolic blood pressure was also lower in adolescents (70.7 mmHg vs 75.8 mmHg, p < 0.001). Glucose intolerance (12.0% vs 19.3%) and insulin resistance (18.2% vs 17.7%) were similar in both groups (p > 0.05, for comparisons). Impaired fasting glucose was lower in adolescents (1.8% vs 11.6%, p = 0.015). Total cholesterol and low-density lipoprotein cholesterol were lower in adolescents (p < 0.001). MS in adolescents and adults were found in 10.3% and 27.8%, respectively (p = 0.005). Visceral adiposity index (VAI) was a good predictor of MS in both adolescents (OR = 12.2), and adults (OR = 9.7).
Conclusions
Most biomarkers of glucose metabolism abnormalities were similar in adolescents and adults with PCOS. The prevalence of MS was lower in adolescents. VAI was a strong predictor of metabolic syndrome, both in adolescent and adult women with PCOS.


Similar content being viewed by others
References
Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO (2004) The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab 89:2745–2749. https://doi.org/10.1210/jc.2003-032046
March WA, Moore VM, Wilson KJ, Phillips DIW, Norman RJ, Davies MJ (2010) The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod 25:544–551. https://doi.org/10.1093/humrep/dep399
Hashemipour M, Faghihimani S, Zolfaghary B, Hovsepian S, Ahmadi F, Haghighi S (2004) Prevalence of polycystic ovary syndrome in girls aged 14–18 years in Isfahan. Iran Horm Res 62:278–282. https://doi.org/10.1159/000081842
Christensen SB, Black MH, Smith N, Martinez MM, Jacobsen SJ, Porter AH, Koebnick C (2013) Prevalence of polycystic ovary syndrome in adolescents. Fertil Steril 100:470–477. https://doi.org/10.1016/j.fertnstert.2013.04.001
Singh A, Vijaya K, Laxmi KS (2018) Prevalence of polycystic ovary syndrome among adolescent girls: a prospective study. Int J Reprod Contracept Obstet Gynecol 7:4375–4378
Carmina E, Oberfield SE, Lobo RA (2010) The diagnosis of polycystic ovary syndrome in adolescents. Am J Obstet Gynecol 203:201.e1-201.e2015. https://doi.org/10.1016/j.ajog.2010.03.008
Witchel SF, Oberfield S, Rosenfield RL, Codner E, Bonny A, Ibáñez L, Pena A, Horikawa R, Gomez-Lobo V, Joel D, Tfayli H, Arslanian S, Dabadghao P, Garcia Rudaz C, Lee PA. The diagnosis of polycystic ovary syndrome during adolescence (2015). Horm Res Paediatr. https://doi.org/10.1159/000375530
Brewer M, Pawelczak M, Kessler M, Shah B (2010) A review of polycystic ovarian syndrome in adolescents. Minerva Pediatr 62:459–473
Gambineri A, Fanelli F, Prontera O, Repaci A, Di Dalmazi G, Zanotti L, Pagotto U, Flacco ME, Guidi J, Fava GA, Manzoli L, Pasquali R (2013) Prevalence of hyperandrogenic states in late adolescent and young women: epidemiological survey on italian high-school students. J Clin Endocrinol Metab 98:1641–1650. https://doi.org/10.1210/jc.2012-3537
Venturoli S, Porcu E, Fabbri R, Pluchinotta V, Ruggeri S, Macrelli S, Paradisi R, Flamigni C (1995) Longitudinal change of sonographic ovarian aspects and endocrine parameters in irregular cycles of adolescence. Pediatr Res 38:974–980. https://doi.org/10.1203/00006450-199512000-00024
Rosenfield RL, Ghai K, Ehrmann DA, Barnes RB (2000) Diagnosis of the polycystic ovary syndrome in adolescence: comparison of adolescent and adult hyperandrogenism. J Pediatr Endocrinol Metab 13:1285–1289
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ, International PCOS Network (2018) Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril 110:364–379. https://doi.org/10.1016/j.fertnstert.2018.05.004
Zore T, Lizneva D, Brakta S, Walker W, Suturina L, Azziz R (2019) Minimal difference in phenotype between adolescents and young adults with polycystic ovary syndrome. Fertil Steril 111:389–396. https://doi.org/10.1016/j.fertnstert.2018.10.020
Coviello AD, Legro RS, Dunaif A (2006) Adolescent girls with polycystic ovary syndrome have an increased risk of the metabolic syndrome associated with increasing androgen levels independent of obesity and insulin resistance. J Clin Endocrinol Metab 91:492–497. https://doi.org/10.1210/jc.2005-1666
de Medeiros SF, Yamamoto MMW, Souto de Medeiros MA, Barbosa BB, Soares JM, Baracat EC (2020) Changes in clinical and biochemical characteristics of polycystic ovary syndrome with advancing age. Endocr connect 9:74–89. https://doi.org/10.1530/EC-19-0496
Fraser IS, Critchley HO, Broder M, Munro MG (2011) The FIGO recommendations on terminologies and definitions for normal and abnormal uterine bleeding. Sem Reprod Med 29:383–390. https://doi.org/10.1055/s-0031-1287662
Sultan C, Paris F (2006) Clinical expression of polycystic ovary syndrome in adolescent girls. Fertil Steril 86:S6. https://doi.org/10.1016/j.fertnstert.2006.04.015
Peña AS, Witchel SF, Hoeger KM, Oberfield SE, Vogiatzi MG, Misso M, Garad R, Dabadghao P, Teede H (2020) Adolescent polycystic ovary syndrome according to the international evidence-based guideline. BMC Med 18:72. https://doi.org/10.1186/s12916-020-01516-x
WHO Consultation on Obesity (1997): Geneva, Switzerland), World Health Organization. Division of Noncommunicable Diseases & World Health Organization. Programme of Nutrition, Family and Reproductive Health (1998). Obesity: preventing and managing the global epidemic: report of a WHO Consultation on Obesity, Geneva, 3–5 June 1997. World Health Organization. https://apps.who.int/iris/handle/10665/63854. Accessed 02 July 2020
SBMIC 2.7 (2014 – 2020). Calculate your BMI correctly rated according to age and sex. https://www.smartbmicalculator.com. Accessed 02 July 2020
Kristensen SL, Ramlau-Hansen CH, Ernst E, Olsen SF, Bonde JP, Vested A, Toft G (2010) A very large proportion of young Danish women have polycystic ovaries: is a revision of the Rotterdam criteria needed? Hum Reprod 25:3117–3122. https://doi.org/10.1093/humrep/deq273
de Medeiros SF, Barbosa JS, Yamamoto MMW (2015) Comparison of steroidogenic pathways among normoandrogenic and hyperandrogenic polycystic ovary syndrome patients and normal cycling women. J Obstet Gynaecol Res 2015(41):254–263. https://doi.org/10.1111/jog.12524
Carmina E, Bucchieri S, Esposito A, Del Puente A, Mansueto P, Orio F, Di Fede G, Rini G (2007) Abdominal fat quantity and distribution in women with polycystic ovary syndrome and extent of its relation to insulin resistance. J Clin Endocrinol Metab 92:2500–2505. https://doi.org/10.1210/jc.2006-2725
Geloneze B, Vasques AC, Stabe CF, Pareja JC, Rosado LE, Queiroz EC, Tambascia MA, Investigators BRAMS (2009) HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian metabolic syndrome study (BRAMS). Arq Bras Endocrinol Metab 53:281–287. https://doi.org/10.1590/s0004-27302009000200020
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. J Pediatr 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Cook S, Auinger P, Li C, Ford ES (2008) Metabolic syndrome rates in United States adolescents, from the national health and nutrition examination survey, 1999–2002. J Pediatr 152:165–170. https://doi.org/10.1016/j.jpeds.2007.06.004
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106:3143–3421
James WPT (1976). Research on obesity. A repot of the DHSS/MRC group. Her Majesty’s Stationary. Department of Health and Social Security and Medical Research Council Group. In: (ed). Hher Majesty’s Stationary Office. London: Office. 94. https://doi.org/10.1111/j.1467-3010.1977.tb00966.x
Amato MC, Giordano C (2014) Visceral adiposity index: an indicator of adipose tissue dysfunction. Int J Endocrinol 3:730827. https://doi.org/10.1155/2014/730827
Kahn HS, Valdez R (2003) Metabolic risks identified by the combination of enlarged waist and elevated triacylglycerol concentration. Am J Clin Nutr 78:928–934. https://doi.org/10.1093/ajcn/78.5.928
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimations of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Diabetes Trial Unit. (2013). The Oxford Centre for Diabetes, Endocrinology and Metabolism [internet]. Oxford, UK: Oxford University; May 1. https://www.dtu.ox.ac.uk/homacalculator. Accessed 02 July 2020
Merino PM, Villarroel C, Jesam C, López P, Codner E (2017) New diagnostic criteria of polycystic ovarian morphology for adolescents: impact on prevalence and hormonal profile. Horm Res Paediatr 88:401–407. https://doi.org/10.1159/000481532
Bellver J, Rodríguez-Tabernero L, Robles A, Muñoz E, Martínez F, Landeras J et al (2018) Group of interest in Reproductive Endocrinology (GIER) of the Spanish fertility society (SEF). Polycystic ovary syndrome throughout a woman’s life. J Assist Reprod Genet 35:25–39. https://doi.org/10.1007/s10815-017-1047-7
Wang JG, Zhang Y, Chen HE, Li Y, Cheng XG, Xu L et al (2013) Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Condition Res 27:236–243. https://doi.org/10.1519/JSC.0b013e31824f2040
Bil E, Dilbaz B, Cirik DA, Ozelci R, Ozkaya E, Dilbaz S (2016) Metabolic syndrome and metabolic risk profile according to polycystic ovary syndrome phenotype. J Obstet Gynaecol Res 42:837–843. https://doi.org/10.1111/jog.12985
Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, Welt CK, Endocrine Society (2013) Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 98:4565–4592. https://doi.org/10.1210/jc.2013-2350
Fernandes AR, de Sá Rosa e Silva AC, Romão GS, Pata MC, dos Reis RM (2005). Insulin resistance in adolescents with menstrual irregularities. J Pediatr Adolesc Gynecol 18:269-274. https://doi.org/10.1016/j.jpag.2005.05.006
Rosenfield RL (2015) The diagnosis of polycystic ovary syndrome in adolescents. Pediatrics 136:1154–1165. https://doi.org/10.1542/peds.2015-1430
Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen OE, Legro RS, Norman RJ, Taylor AE, Witchel SF, Androgen Excess Society (2006) Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an androgen excess society guideline. J Clin Endocrinol Metab 91:4237–4245. https://doi.org/10.1210/jc.2006-0178
Galobardes B, Davey Smith G, Jefferys M, McCarron P, Cohort GA (2005) Has acne increased? Prevalence of acne history among university students between 1948 and 1968. The Glasgow Alumni Cohort Study. Br J Dermatol 152:824–825. https://doi.org/10.1111/j.1365-2133.2005.06527.x
Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen OE, Legro RS, Norman RJ, Taylor AE, Witchel SF, Task Force on the Phenotype of the Polycystic Ovary Syndrome of The Androgen Excess and PCOS Society (2009) The androgen excess and PCOS society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril 91:456–488. https://doi.org/10.1016/j.fertnstert.2008.06.035
Fruzzetti F, Perini D, Lazzarini V, Parrini D, Genazzani AR (2009) Adolescent girls with polycystic ovary syndrome showing different phenotypes have a different metabolic profile associated with increasing androgen levels. Fertil Steril 92:626–634. https://doi.org/10.1016/j.fertnstert.2008.06.004
Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E (2015) American Association of clinical endocrinologists, American college of endocrinology, and androgen excess and PCOS society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome - part 2. Endocr Pract 21:1415–1426. https://doi.org/10.4158/EP15748.DSCPT2
Hickey M, Sloboda DM, Atkinson HC, Doherty DA, Franks S, Norman RJ, Newnham JP, Hart R (2009) The relationship between maternal and umbilical cord androgen levels and polycystic ovary syndrome in adolescence: a prospective cohort study. J Clin Endocrinol Metab 94:3714–3720. https://doi.org/10.1210/jc.2009-0544
Villarroel C, Merino PM, López P, Eyzaguirre FC, Van Velzen A, Iñiguez G, Codner E (2011) Polycystic ovarian morphology in adolescents with regular menstrual cycles is associated with elevated anti-Mullerian hormone. Hum Reprod 26:2861–2868. https://doi.org/10.1093/humrep/der223
Mortensen M, Rosenfield RL, Littlejohn E (2006) Functional significance of polycystic-size ovaries in healthy adolescents. J Clin Endocrinol Metab 91:3786–3790. https://doi.org/10.1210/jc.2006-0835
Dewailly D, Lujan ME, Carmina E, Cedars MI, Laven J, Norman RJ, Escobar-Morreale HF (2020) Definition and significance of polycystic ovarian morphology: a task force report from the Androgen excess and polycystic ovary syndrome society. Hum Reprod Update 20:334–352. https://doi.org/10.1093/humupd/dmt061
Sawathiparnich P, Weerakulwattana L, Santiprabhob J, Likitmaskul S (2005) Obese adolescent girls with polycystic ovary syndrome (PCOS) have more severe insulin resistance measured by HOMA-IR score than obese girls without PCOS. J Med Assoc Thai 88:S33–S37
Pasquali R, Gambineri A (2006) Polycystic ovary syndrome: a multifaceted disease from adolescence to adult age. Ann NY Acad Sci 1092:158–174. https://doi.org/10.1196/annals.1365.014
Leibel NI, Baumann EE, Kocherginsky M, Rosenfield RL (2006) Relationship of adolescent polycystic ovary syndrome to parental metabolic syndrome. J Clin Endocrinol Metab 91:1275–1283. https://doi.org/10.1210/jc.2005-1707
Arslanian SA, Lewy VD, Danadian K (2001) Glucose intolerance in obese adolescents with polycystic ovary syndrome: roles of insulin resistance and beta-cell dysfunction and risk of cardiovascular disease. J Clin Endocrinol Metab 86:66–71. https://doi.org/10.1210/jcem.86.1.7123
Legro RS, Kunselman AR, Dodson WC, Dunaif A (1999) Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab 84:165–169. https://doi.org/10.1210/jcem.84.1.5393
Ehrmann DA, Barnes RB, Rosenfield RL, Cavaghan MK, Imperial J (1999) Prevalence of impaired glucose tolerance and diabetes in women with polycystic ovary syndrome. Diabetes Care 22:141–146. https://doi.org/10.2337/diacare.22.1.141
Palmert MR, Gordon CM, Kartashov AI, Legro RS, Emans SJ, Dunaif A (2002) Screening for abnormal glucose tolerance in adolescents with polycystic ovary syndrome. J Clin Endocrinol Metab 87:1017–1023. https://doi.org/10.1210/jcem.87.3.8305
Alemzadeh R, Kichler J, Calhoun M (2010) Spectrum of metabolic dysfunction in relationship with hyperandrogenemia in obese adolescent girls with polycystic ovary syndrome. Eur J Endocrinol 162:1093–1099. https://doi.org/10.1530/EJE-10-0205
Legro RS, Kunselman AR, Dunaif A (2001) Prevalence and predictors of dyslipidemia in women with polycystic ovary syndrome. Am J Med 111:607–613. https://doi.org/10.1016/s0002-9343(01)00948-2
Demirel F, Bideci A, Cinaz P, Camurdan MO, Biberoğlu G, Yesilkaya E, Hasanoğlu A (2007) Serum leptin, oxidized low density lipoprotein and plasma asymmetric dimethylarginine levels and their relationship with dyslipidaemia in adolescent girls with polycystic ovary syndrome. Clin Endocrinol 67:129–134. https://doi.org/10.1111/j.1365-2265.2007.02849.x
Pedroso DC, Melo AS, Carolo AL, Vieira CS, Rosa e Silva AC, dos Reis RM, (2012) Frequency and risk factors for metabolic syndrome in adolescents and adults women with polycystic ovary syndrome. Rev Bras Ginecol Obstet 34:357–361. https://doi.org/10.1590/s0100-72032012000800003
Vural B, Caliskan E, Turkoz E, Kilic T, Demirci A (2005) Evaluation of metabolic syndrome frequency and premature carotid atherosclerosis in young women with polycystic ovary syndrome. Hum Reprod 20:2409–2413. https://doi.org/10.1093/humrep/dei100
Salley KE, Wickham EP, Cheang KI, Essah PA, Karjane NW, Nestler JE (2007) Glucose intolerance in polycystic ovary syndrome–a position statement of the Androgen Excess Society. J Clin Endocrinol Metab 92:4546–4556. https://doi.org/10.1210/jc.2007-1549
Park HR, Choi Y, Lee HJ, Oh JY, Hong YS, Sung YA (2007) The metabolic syndrome in young Korean women with polycystic ovary syndrome. Diabetes Res Clin Pract 77:S243–S246. https://doi.org/10.1016/j.diabres.2007.01.065
Han Y, Kim HS, Hye-Jin L, Jee-Young O, Yeon-Ah S (2015) Metabolic effects of polycystic ovary syndrome in adolescents. Ann Pediatr Endocrinol Metab 20:136–142. https://doi.org/10.6065/apem.2015.20.3.136
Acknowledgements
The authors are grateful to Liberty Medical Communications, LLC, for English proofreading.
Funding
This research did not receive any specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
SFdM: design, data description, statistical analysis, and writing the manuscript. MASdM: data search, revision of the manuscript. BBB: data search, data analysis, revision of the manuscript. MMWY: data search, revision of the manuscript. GARM: data search, revision of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors fully declare there is either no financial or other conflicts of interest that could be perceived as prejudicing the impartiality of this study.
Ethics approval
A specific signed informed consent document approved by the local Committee for Ethics in Research was not necessary at this time because only the medical records of all patients were reviewed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Medeiros, S.F., de Medeiros, M.A.S., Barbosa, B.B. et al. Comparison of metabolic and obesity biomarkers between adolescent and adult women with polycystic ovary syndrome. Arch Gynecol Obstet 303, 739–749 (2021). https://doi.org/10.1007/s00404-020-05867-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05867-x