Abstract
Purpose
This study aimed to develop a valid and reliable tool for evaluation of sexual health assessment in infertile women.
Methods
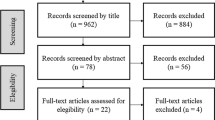
This was a mixed exploratory study consisting of two phases. At phase one, we reviewed the existing instruments and interviewed 20 infertile women to generate an item pool. Then, the research team examined items and invited a panel of experts (n = 15) and a group of infertile women (n = 10) to review the items to establish content and face validity. Accordingly, the provisional version of the questionnaire containing 62 items was provided. At phase two, a cross-sectional study was conducted to evaluate the questionnaire. The structural validity was examined by performing exploratory factor analysis. Internal consistency was estimated by the Cornbach’s alpha coefficient and test–retest analysis was performed to assess stability.
Results
The final questionnaire consisted of 45 items and a total of 372 infertile women completed the questionnaire. The mean age of women was 30.8 (SD 6.0) years and this was 5.6 (SD 4.2) for duration of infertility. The results obtained from exploratory factor analysis indicated a five-factor solution for the questionnaire that jointly explained 51.39% of variance observed. At this stage, 15 items were deleted due to low factor loading. The analysis of internal consistency and stability yielded satisfactory results (Cronbach alpha: 0.93, ICC 0.97, respectively). Further analysis indicated that lower sexual health in infertile women was associated with education (OR for primary education 2.61, 95% CI 1.44–4.76, P = 0.002) and being housewife (OR 2.35, 95% CI 1.15–4.83, P = 0.01).
Conclusion
The findings showed that the Sexual Health Assessment Tool for Infertile Women (SEHAT-IW) is a reliable and valid instrument to assess infertile women’s sexual health.

Similar content being viewed by others
Data availability
The data sets generated and analyzed during this study are not publicly presented because of a desire to protect the participants’ anonymity; they are, however, available from the corresponding author on advisable request.
References
Bennett L (2016) Infertility and inequity across the globe. Asian Popul Stud 13(1):1–4
Zegers-Hochschild F, David Adamson G, Dyer S, Racowsky C, De Mouzon J, Sokol R et al (2017) The international glossary on infertility and fertility care. Fertil Steril 108(3):393–406
Jamali S, Zarei H, Rasekh JA (2014) The relationship between body mass index and sexual function in infertile women: a cross-sectional survey. Iran J Reprod Med 12(3):189–198
Davari Tanha F, Mohseni M, Ghajarzadeh M (2014) Sexual function in women with primary and secondary infertility in comparison with controls. Int J Impot Res 26:132–134
Bokaie M, Simbar M, Yassini Ardekani SM (2015) Sexual behavior of infertile women: a qualitative study. Iran J Reprod Med 13(10):645–656
Berger MH, Messore M, Pastuszak AW, Ramasamy R (2016) Association between infertility and sexual dysfunction in men and women. Sexual Med Rev 4(4):353–365
Slater C, Robinson AJ (2014) Sexual health in adolescents. Clin Dermatol 32(2):189–195
Edwards WM, Coleman E (2004) Defining sexual health: a descriptive overview. Arch Sex Behav 33(3):189–195
Grill E, Schattman G (2016) Female sexual dysfunction and infertility. Management of sexual dysfunction in men and women. Springer, New York, pp 337–342
Kucur Suna K, Ilay G, Aysenur A, Kerem Han G, Eda Ulku U, Pasa U et al (2016) Effects of infertility etiology and depression on female sexual function. J Sex Marital Ther 42(1):27–35
Smith NK, Madeira J, Heather RM (2015) Sexual function and fertility quality of life in women using in vitro fertilization. Sexual Med 12(4):985–993
Gabr A, Omran EF, Abdallah AA, Kotb MM, Farid EZ, Dieb AS et al (2017) Prevalence of sexual dysfunction in infertile versus fertile couples. Eur J Obstet Gynecol Reprod Biol 217:38–43
Momeni KH, Jalilian N, Yazdanbakhsh K, Mokari Z, Rezaei M (2018) Effects of sexual education skills on the treatment outcomes of infertile women. Iran J Obstet Gynecol Infertil 21(3):5–14
Hensel DJ, Dennis Fortenberry JA (2013) Multidimensional model of sexual health and sexual and prevention behavior among adolescent women. J Adolesc Health. 52(2):219–227
Czyżkowska A, Awruk K, Janowski K (2016) Sexual satisfaction and sexual reactivity in infertile women: the contribution of the dyadic functioning and clinical variables. Int J Fertil Steril 4(9):465–476
Graneheim UH, Lundman B (2004) Qualitative content analysis in nursing research concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24(2):105–120
Ramezani MA, Ghaemmaghami A, Talakar M, Saadat SH, Zamani E, Shams J et al (2013) Validity and reliability assessment of multi-dimensional sexual self-concept questionnaire for Iranian population. Iran J Mil Med 14(4):302–309
Farokhi S, Shareh H (2014) Psychometric properties of the Persian version of the sexual self-esteem index for woman-SHort Form. Iran J Psychiatry Clin Psychol 20(3):252–263
Maasoumi R (2014) Exploring the concept of female quality of sexual life, factors and dimensions: development and psychometric properties of a cultural-based instrument, in Faculty of Medical Sciences. Tarbiat Modares University, Tehran, p 284
Hair Jr, Joseph F, William CB, Barry JB, Rolph EA (2014) Multivariate data analysis, 7th edn. Pearson, Harlow, Essex, United Kingdom
Plichta SB, Kelvin E (2012) Munro’s statistical methods for health care research, 3rd edn. Jame-e-Negar, Tehran, p 556
Waltz CF, Strickland OL, Lenz ER (2010) Measurement in nursing and health research, F. Springer Publishing Company, New York, p 505
Shahraki Z, Davari Tanha F, Ghajarzadeh M (2018) Depression, sexual dysfunction and sexual quality of life in women with infertility. BMC Women’s Health. 18(92):1–4
Moghasemi S (2017) Development and psychometric assessment of female midlife sexual health instrument, in School of Nursing and Midwifery. Shahid Beheshti University of medical sciences, Tehran, p 215
Luara CF (2007) A mixed methods analysis of the concept of female sexual health, in Department of Interdisciplinary Health Studies. Western Michigan University, Kalamazoo, pp 1–271
Rosen RC, Bachmann GA, Reese JB, Gentner L, Leiblum S, Wajszczuk CH, Wanser R (2009) Female sexual well-being scale (FSWB scale): development and psychometric validation in sexually functional women. J Sexual Med 6(5):1297–1305
Brotto L, Atallah S, Johnson-Agbakwu C, Rosenbaum T, Abdo C, Byers ES et al (2016) Psychological and interpersonal dimensions of sexual function and dysfunction. J Sexual Med. 13:538–571
Direkvand-Moghadam A, Delpisheh A, Direkvand-Moghadam A (2015) Effect of infertility on sexual function: a cross-sectional study. J Clin Diagn Res 9(5):QC01
Kohan SH, Ghasemi Z, Beigi M (2015) Exploring infertile women’s experiences about sexual life: a qualitative study. Iran J Nurs Midwifery Res 20(1):34–39
Jafarzadeh-Kenarsar F, Ghahiri A, Habib M, Zargham-Boroujen A (2015) Exploration of infertile couples’ support requirements: a qualitative study. Int J Fertil Steril 9(1):81–92
Hasanpour SH, Bani S, Mirghafourvand M, Yahyavi KF (2014) Mental health and its personal and social predictors in infertile women. J Caring Sci 3(1):37–45
Thomas HN, Thurston RC (2016) A biopsychosocial approach to women’s sexual function and dysfunction at midlife: a narrative review. Maturitas 87:49–60
Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E et al (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (project Leonardo). Vasc Health Risk Manag 6:297–305
Acknowledgements
This study is part of a Ph.D. dissertation approved by the Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran. The authors would like to acknowledge all the participants (infertile women) who took part in this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
SHJ involved in the study design, analysis, and interpretation of data and critically revised the final manuscript. ZD collected the data and drafted the manuscript. AK and FA contributed to the statistics and critically revised the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Ethics Committee of Tarbiat Modares University (IR.TMU.REC.1396.659). The present study only involved persons who gave their informed consent. For this, verbal informed consent was obtained from all participants before the start of the study, and all members of the participants completed informed written consent after being informed about the aims of the research. The designed questionnaire was distributed among the participants, while they remained anonymous; there was no private information that could enable the association of any answers with any of the persons in the present study. To protect the rights and interests of all participants, no records of consent by name were kept. Each completed instrument was given to the research fellow on the same day of data collection.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Daneshfar, Z., Sadatmahalleh, S.J., Kazemnejad, A. et al. Development and psychometric evaluation of the Sexual Health Assessment Tool for Infertile Women (SEHAT-IW). Arch Gynecol Obstet 303, 589–596 (2021). https://doi.org/10.1007/s00404-020-05832-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05832-8