Abstract
Purpose
The etiology of endometriosis is mostly under-explored, but abnormalities in the immune system leading to an autoimmune reaction have been suggested. The systemic lupus erythematosus (SLE) is one of the most common autoimmune diseases. The purpose of this study was to investigate the risk of SLE in patients with endometriosis.
Methods
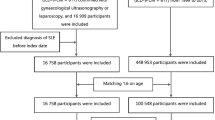
A total of 17,779 patients with endometriosis and 17,779 controls (without endometriosis) matched by age, index year, and Charlson Comorbidity Index (CCI) score were enrolled between 2000 and 2012. Patients were then followed until the end of 2013 using Taiwan’s National Health Insurance Research Database, at which time participants who developed SLE were identified. Cox regression analysis was used to calculate the hazard ratio (HR) with a 95% confidence interval (CI) of SLE incidence rate between patients with endometriosis and unaffected controls.
Results
After adjusting for age, CCI score, and different treatment options, patients with endometriosis were at increased risk of SLE compared to unaffected controls (0.85 versus 0.57 per 1000 person-years, HR 1.86, 95% CI 1.36–2.53). Also, higher baseline CCI scores (CCI score 1–2 and ≥ 3 vs. 0—HR 2.33–4.98) were at increased risk of SLE. During follow-up, hormonal treatment for endometriosis could reduce the risk of SLE (short-term and long-term vs. non-use HR 0.48–0.62), while surgical treatment appeared to have a limited impact on the risk of SLE.
Conclusion
Patients with endometriosis were at increased risk of SLE, and adequate hormonal treatment could reduce the risk of SLE, providing a reference for developing prevention interventions.

Similar content being viewed by others
References
Zondervan KT, Becker CM, Koga K, Missmer SA, Taylor RN, Vigano P (2018) Endometriosis. Nat Rev Dis Primers 4(1):9. https://doi.org/10.1038/s41572-018-0008-5
Zhang T, De Carolis C, Man GCW, Wang CC (2018) The link between immunity, autoimmunity and endometriosis: a literature update. Autoimmun Rev 17(10):945–955. https://doi.org/10.1016/j.autrev.2018.03.017
Lisnevskaia L, Murphy G, Isenberg D (2014) Systemic lupus erythematosus. Lancet 384(9957):1878–1888. https://doi.org/10.1016/S0140-6736(14)60128-8
Catalina MD, Owen KA, Labonte AC, Grammer AC, Lipsky PE (2019) The pathogenesis of systemic lupus erythematosus: Harnessing big data to understand the molecular basis of lupus. J Autoimmun. https://doi.org/10.1016/j.jaut.2019.102359
Barbhaiya M, Costenbader KH (2016) Environmental exposures and the development of systemic lupus erythematosus. Curr Opin Rheumatol 28(5):497–505. https://doi.org/10.1097/BOR.0000000000000318
Shigesi N, Kvaskoff M, Kirtley S, Feng Q, Fang H, Knight JC, Missmer SA, Rahmioglu N, Zondervan KT, Becker CM (2019) The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Hum Reprod Update 25(4):486–503. https://doi.org/10.1093/humupd/dmz014
Nielsen NM, Jorgensen KT, Pedersen BV, Rostgaard K, Frisch M (2011) The co-occurrence of endometriosis with multiple sclerosis, systemic lupus erythematosus and Sjogren syndrome. Hum Reprod 26(6):1555–1559. https://doi.org/10.1093/humrep/der105
Harris HR, Costenbader KH, Mu F, Kvaskoff M, Malspeis S, Karlson EW, Missmer SA (2016) Endometriosis and the risks of systemic lupus erythematosus and rheumatoid arthritis in the Nurses’ Health Study II. Ann Rheum Dis 75(7):1279–1284. https://doi.org/10.1136/annrheumdis-2015-207704
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Bianco B, Andre GM, Vilarino FL, Peluso C, Mafra FA, Christofolini DM, Barbosa CP (2012) The possible role of genetic variants in autoimmune-related genes in the development of endometriosis. Hum Immunol 73(3):306–315. https://doi.org/10.1016/j.humimm.2011.12.009
Tizaoui K, Kim SH, Jeong GH, Kronbichler A, Lee KS, Lee KH, Shin JI (1858C) Association of PTPN22 1858C/T polymorphism with autoimmune diseases: a systematic review and bayesian approach. J Clin Med. https://doi.org/10.3390/jcm8030347
Sharif K, Watad A, Coplan L, Lichtbroun B, Krosser A, Lichtbroun M, Bragazzi NL, Amital H, Afek A, Shoenfeld Y (2018) The role of stress in the mosaic of autoimmunity: an overlooked association. Autoimmun Rev 17(10):967–983. https://doi.org/10.1016/j.autrev.2018.04.005
Costenbader KH, Feskanich D, Stampfer MJ, Karlson EW (2007) Reproductive and menopausal factors and risk of systemic lupus erythematosus in women. Arthritis Rheum 56(4):1251–1262. https://doi.org/10.1002/art.22510
Lateef A, Petri M (2012) Hormone replacement and contraceptive therapy in autoimmune diseases. J Autoimmun 38(2–3):J170–176. https://doi.org/10.1016/j.jaut.2011.11.002
Kuo CF, Chou IJ, Rees F, Grainge MJ, Lanyon P, Davenport G, Mallen CD, Chung TT, Chen JS, Zhang W, Doherty M (2019) Temporal relationships between systemic lupus erythematosus and comorbidities. Rheumatology (Oxford) 58(5):840–848. https://doi.org/10.1093/rheumatology/key335
Acknowledgements
The authors thank Shinn-Zong Lin for cross-hospital integration.
Funding
This study is supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004); MOST Clinical Trial Consortium for Stroke, Taiwan (MOST 108-2321-B-039-003); Tseng-Lien Lin Foundation, Taichung, Taiwan. The funding source has no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
YHL and SFC managed the literature searches and wrote the introduction of the manuscript. YCY and CYH did all the analyses and wrote the method and results of the manuscript. YCS conceived the study and wrote the discussion of the manuscript. All authors have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The Institutional Review Board of China Medical University approved this study (CMUH104-REC2-115). All research methods were carried out following guidelines and regulations.
Informed consent
Since the NHIRD only contains anonymized secondary data, the need for informed consent from individual subjects has been lifted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, YH., Yang, YC., Chen, SF. et al. Risk of systemic lupus erythematosus in patients with endometriosis: A nationwide population-based cohort study. Arch Gynecol Obstet 302, 1197–1203 (2020). https://doi.org/10.1007/s00404-020-05726-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05726-9