Abstract
Purpose
Intraamniotic infection, categorized into isolated maternal fever, suspected intraamniotic infection (SII), and confirmed intraamniotic infection, is associated with neonatal morbidity. However, there is paucity of data regarding the association between intraamniotic infection duration and neonatal outcomes among term singleton vaginal deliveries. We aimed to study the risk factors for adverse neonatal outcome among vaginal deliveries complicated by SII.
Methods
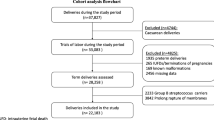
A retrospective observational study conducted at a tertiary medical center. All consecutive singleton term deliveries with SII were included between 2011 and 2019. Maternal and obstetrical characteristics were evaluated to identify risk factors for adverse neonatal outcome. Correlation between SII duration and neonatal adverse outcome was analyzed.
Results
Overall, 882 were analyzed. Most women (85.4%) were primiparous. Median gestation age at delivery was 40 2/7 weeks. Median time from SII to delivery was 170 min. Adverse neonatal outcomes occurred in 113 (12.8%) of deliveries. Duration of SII was not associated with adverse neonatal outcome. Analysis for determinants of adverse neonatal outcome revealed that oligohydramnios was more common in pregnancies with adverse neonatal outcome (7/113 (6.2%) vs. 41 (5.4%) OR [95% CI] 2.47 (1.02–5.98), p = 0.03). Duration of second stage of labor was longer in the adverse outcome group (median 179 min vs. 126 min, p = 0.008). Prolonged second stage was more common in the adverse outcome group (60 (53.1%) vs. 273 (35.5%) OR [95% CI] 2.05 (1.38–3.06), p < 0.001). On logistic regression analysis, prolonged second stage was the only modifiable factor independently associated with adverse neonatal outcome [adjusted OR 2.09 (1.37–3.2), p = 0.001]. Other variables tested did not differ between groups.
Only phototherapy and base excess ≥ 12 mmol/L were significantly associated with the duration of second stage of labor; for each additional hour of the second stage, the OR for the former increased by 0.34 (p = 0.008), and for the latter by 0.69 (p = 0.007).
Conclusion
Duration of suspected intraamniotic infection was not associated with increased neonatal morbidity among women delivering vaginally at term. Prolonged second stage was a strong independent predictor of an adverse neonatal outcome among fetuses exposed to intraamniotic infection.

Similar content being viewed by others
Abbreviations
- SII:
-
Suspected intraamniotic infection
References
ACOG Practice (2017) Committee opinion no. 712: intrapartum management of intraamniotic infection. Obstet Gynecol 130(2):e95–e101
Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K et al (2016) Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol 127(3):426–436
Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, Kim YM (2015) Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol 213(4 Suppl):S29–52
Escobar GJ, Puopolo KM, Wi S, Turk BJ, Kuzniewicz MW, Walsh EM et al (2014) Stratification of risk of early-onset sepsis in newborns ≥ 34 weeks’ gestation. Pediatrics 133(1):30–36
Rouse DJ, Landon M, Leveno KJ, Leindecker S, Varner MW, Caritis SN et al (2004) The maternal-fetal medicine units cesarean registry: chorioamnionitis at term and its duration-relationship to outcomes. Am J Obstet Gynecol 191(1):211–216
Venkatesh KK, Glover AV, Vladutiu CJ, Stamilio DM (2019) Association of chorioamnionitis and its duration with adverse maternal outcomes by mode of delivery: a cohort study. BJOG 126(6):719–727
Venkatesh KK, Jackson W, Hughes BL, Laughon MM, Thorp JM, Stamilio DM (2019) Association of chorioamnionitis and its duration with neonatal morbidity and mortality. J Perinatol 39(5):673–682
Impey L, Greenwood C, MacQuillan K, Reynolds M, Sheil O (2001) Fever in labour and neonatal encephalopathy: a prospective cohort study. BJOG 108(6):594–597
Greenwell EA, Wyshak G, Ringer SA, Johnson LC, Rivkin MJ, Lieberman E (2012) Intrapartum temperature elevation, epidural use, and adverse outcome in term infants. Pediatrics 129(2):e447–e454
Newton ER (1993) Chorioamnionitis and intraamniotic infection. Clin Obstet Gynecol 36(4):795–808
Soper DE, Mayhall CG, Dalton HP (1989) Risk factors for intraamniotic infection: a prospective epidemiologic study. Am J Obstet Gynecol 161(3):562–566 (discussion 6–8)
Tran SH, Caughey AB, Musci TJ (2003) Meconium-stained amniotic fluid is associated with puerperal infections. Am J Obstet Gynecol 189(3):746–750
Gibbs RS, Dinsmoor MJ, Newton ER, Ramamurthy RS (1988) A randomized trial of intrapartum versus immediate postpartum treatment of women with intra-amniotic infection. Obstet Gynecol 72(6):823–828
Gynecologists ACoOa, Pregnancy TFoHi (2013) Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol 122(5):1122–1131
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 144(7):768–773
Alexander JM, McIntire DM, Leveno KJ (1999) Chorioamnionitis and the prognosis for term infants. Obstet Gynecol 94(2):274–278
Caughey AB, Cahill AG, Guise JM, Rouse DJ, ACoOaG (College), Medicine SfM-F (2014) Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 210(3):179–193
Naveiro-Fuentes M, Puertas Prieto A, Ruíz RS, Carrillo Badillo MP, Ventoso FM, Gallo Vallejo JL (2016) Perinatal outcomes with isolated oligohydramnios at term pregnancy. J Perinat Med 44(7):793–798
Rossi AC, Prefumo F (2013) Perinatal outcomes of isolated oligohydramnios at term and post-term pregnancy: a systematic review of literature with meta-analysis. Eur J Obstet Gynecol Reprod Biol 169(2):149–154
Chauhan SP, Hendrix NW, Morrison JC, Magann EF, Devoe LD (1997) Intrapartum oligohydramnios does not predict adverse peripartum outcome among high-risk parturients. Am J Obstet Gynecol 176(6):1130–1136 (discussion 6–8)
Hasegawa J, Matsuoka R, Ichizuka K, Kotani M, Ohmori A, Nakamura M et al (2008) Intrapartum fetal heart rate pattern in oligohydramnios. Fetal Diagn Ther 24(3):267–270
Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK (2014) Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol 124(1):57–67
Bailit JL, Grobman WA, Rice MM, Wapner RJ, Reddy UM, Varner MW et al (2016) Evaluation of delivery options for second-stage events. Am J Obstet Gynecol 214(5):638e1–638e10
Hauth JC, Gilstrap LC, Hankins GD, Connor KD (1985) Term maternal and neonatal complications of acute chorioamnionitis. Obstet Gynecol 66(1):59–62
Funding
No external funding was used in this conduct of this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript. GL, RM and AR reviewed the literature and wrote the paper. AT, DS, TC and RK performed the procedures and collected the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required and was waived by the institutional review board approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key message: Duration of suspected intraamniotic infection is not associated with increased neonatal morbidity among women delivering vaginally at term.
Rights and permissions
About this article
Cite this article
Levin, G., Rottenstreich, A., Tsur, A. et al. Determinants of adverse neonatal outcome in vaginal deliveries complicated by suspected intraamniotic infection. Arch Gynecol Obstet 302, 1345–1352 (2020). https://doi.org/10.1007/s00404-020-05717-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05717-w