Abstract
Purpose
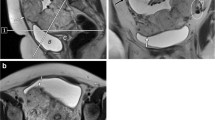
To assess the value of various grey-scale ultrasound, 2D color Doppler, and 3D power Doppler sonographic markers in predicting major intraoperative blood loss during planned cesarean hysterectomy for cases diagnosed with placenta accreta spectrum (PAS) disorders.
Methods
50 women diagnosed with PAS were scanned the day before planned delivery and hysterectomy for various sonographic markers indicative of placental invasion. These women were then later divided according to blood loss in two groups: group A (minor hemorrhage, < 2500 ml), and group B (major hemorrhage, > 2500 ml), and the data were analyzed.
Results
The odds ratio (OR) for major hemorrhage was as follows for the following sonographic markers: ‘number of lacunae > 4′ OR 3.8 95% CI (1.0–13.8) (p = 0.047); ‘subplacental hypervascularity’ OR 10.8 95% CI (1.2–98.0) (p = 0.035); ‘tortuous vascularity with ‘chaotic branching’ OR 10.8 95%CI (1.2–98.0) (p = 0.035); ‘numerous coherent vessels involving the serosa–bladder interface OR 14.6 95% CI (2.7–80.5) (p = 0.002); and ‘presence of bridging vessels OR 2.9 95% CI (1.4–6.9) (p = 0.005). Only the presence of numerous coherent vessels involving the bladder–serosal interface (p = 0.002) was proven to be independent predictor of major hemorrhage during hysterectomy.
Conclusion
The use of 2D color Doppler and 3D power Doppler can help predict massive hemorrhage in cases of PAS disorders.







Similar content being viewed by others
Abbreviations
- AIP:
-
Abnormally invasive placenta
- PAS:
-
Placenta accreta spectrum
- PRBCs:
-
Packed red blood cells
- RBCs:
-
Red blood cells
References
Gielchinsky Y, Rojansky N, Fasouliotis SJ, Ezra Y (2002) Placenta accreta–summary of 10 years: a survey of 310 cases. Placenta 23(2–3):210–214. https://doi.org/10.1053/plac.2001.0764
Luke RK, Sharpe JW, Greene RR (1966) Placenta accreta: the adherent or invasive placenta. Am J Obstet Gynecol 95(5):660–668. https://doi.org/10.1016/s0002-9378(16)34741-x
Jauniaux E, Ayres-de-Campos D (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: introduction. Int J Gynaecol Obstet Off Org Int Feder Gynaecol Obstet 140(3):261–264. https://doi.org/10.1002/ijgo.12406
Esh-Broder E, Ariel I, Abas-Bashir N, Bdolah Y, Celnikier DH (2011) Placenta accreta is associated with IVF pregnancies: a retrospective chart review. BJOG Int J Obstet Gynaecol 118(9):1084–1089. https://doi.org/10.1111/j.1471-0528.2011.02976.x
(2017) Prevention and management of postpartum haemorrhage: green-top guideline No. 52. BJOG: Int J Obstet Gynaecol 124 (5):e106-e149. https://doi.org/10.1111/1471-0528.14178
Eller AG, Porter TF, Soisson P, Silver RM (2009) Optimal management strategies for placenta accreta. BJOG Int J Obstet Gynaecol 116(5):648–654. https://doi.org/10.1111/j.1471-0528.2008.02037.x
(2012) Committee opinion no. 529: placenta accreta. Obstetr Gynecol 120 (1):207–211. https://doi.org/10.1097/AOG.0b013e318262e340
Thia EW, Lee SL, Tan HK, Tan LK (2007) Ultrasonographical features of morbidly-adherent placentas. Singap Med J 48(9):799–802 (quiz 803)
Shih JC, Palacios Jaraquemada JM, Su YN, Shyu MK, Lin CH, Lin SY, Lee CN (2009) Role of three-dimensional power Doppler in the antenatal diagnosis of placenta accreta: comparison with gray-scale and color Doppler techniques. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 33(2):193–203. https://doi.org/10.1002/uog.6284
Collins SL, Stevenson GN, Al-Khan A, Illsley NP, Impey L, Pappas L, Zamudio S (2015) Three-dimensional power Doppler ultrasonography for diagnosing abnormally invasive placenta and quantifying the risk. Obstet Gynecol 126(3):645–653. https://doi.org/10.1097/aog.0000000000000962
Collins SL, Ashcroft A, Braun T, Calda P, Langhoff-Roos J, Morel O, Stefanovic V, Tutschek B, Chantraine F (2016) Proposal for standardized ultrasound descriptors of abnormally invasive placenta (AIP). Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 47(3):271–275. https://doi.org/10.1002/uog.14952
Wong HS, Cheung YK, Zuccollo J, Tait J, Pringle KC (2008) Evaluation of sonographic diagnostic criteria for placenta accreta. J Clin Ultrasound JCU 36(9):551–559. https://doi.org/10.1002/jcu.20524
Fukushima K, Fujiwara A, Anami A, Fujita Y, Yumoto Y, Sakai A, Morokuma S, Wake N (2012) Cervical length predicts placental adherence and massive hemorrhage in placenta previa. J Obstet Gynaecol Res 38(1):192–197. https://doi.org/10.1111/j.1447-0756.2011.01669.x
Hussein AM, Kamel A, Raslan A, Dakhly DMR, Abdelhafeez A, Nabil M, Momtaz M (2019) Modified cesarean hysterectomy technique for management of cases of placenta increta and percreta at a tertiary referral hospital in Egypt. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-018-5027-7
Kamel A, El-Mazny A, Salah E, Ramadan W, Hussein AM, Hany A (2018) Manual removal versus spontaneous delivery of the placenta at cesarean section in developing countries: a randomized controlled trial and review of literature. J Matern Fetal Neonatal Med. 31(24):3308–3313. https://doi.org/10.1080/14767058.2017.1369522
(2015) Quantification of blood loss: AWHONN practice brief number 1. J Obstet Gynecol Neonatal Nurs JOGNN 44(1):158–160. https://doi.org/10.1111/1552-6909.12519
Guasch E, Gilsanz F (2016) Massive obstetric hemorrhage: current approach to management. Med Intensiva 40(5):298–310. https://doi.org/10.1016/j.medin.2016.02.010
Girard T, Mortl M, Schlembach D (2014) New approaches to obstetric hemorrhage: the postpartum hemorrhage consensus algorithm. Curr Opin Anaesthesiol 27(3):267–274. https://doi.org/10.1097/aco.0000000000000081
Collis RE, Collins PW (2015) Haemostatic management of obstetric haemorrhage. Anaesthesia. https://doi.org/10.1111/anae.12913(70 Suppl 1:78-86, e27-78)
Chan YH (2003) Biostatistics 102: quantitative data–parametric and non-parametric tests. Singap Med J 44(8):391–396
Chan YH (2003) Biostatistics 103: qualitative data: tests of independence. Singap Med J 44(10):498–503
Chan YH (2004) Biostatistics 202: logistic regression analysis. Singap Med J 45(4):149–153
Wu S, Kocherginsky M, Hibbard JU (2005) Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol 192(5):1458–1461. https://doi.org/10.1016/j.ajog.2004.12.074
Warshak CR, Ramos GA, Eskander R, Benirschke K, Saenz CC, Kelly TF, Moore TR, Resnik R (2010) Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet Gynecol 115(1):65–69. https://doi.org/10.1097/AOG.0b013e3181c4f12a
Angstmann T, Gard G, Harrington T, Ward E, Thomson A, Giles W (2010) Surgical management of placenta accreta: a cohort series and suggested approach. Am J Obstet Gynecol 202(1):38.e31–39. https://doi.org/10.1016/j.ajog.2009.08.037
Asicioglu O, Sahbaz A, Gungorduk K, Yildirim G, Asicioglu BB, Ulker V (2014) Maternal and perinatal outcomes in women with placenta praevia and accreta in teaching hospitals in Western Turkey. J Obstet Gynaecol J Inst Obstet Gynaecol 34(6):462–466. https://doi.org/10.3109/01443615.2014.902040
Clark SL, Phelan JP, Yeh SY, Bruce SR, Paul RH (1985) Hypogastric artery ligation for obstetric hemorrhage. Obstet Gynecol 66(3):353–356
Chong Y, Zhang A, Wang Y, Chen Y, Zhao Y (2018) An ultrasonic scoring system to predict the prognosis of placenta accreta: a prospective cohort study. Medicine 97(35):e12111. https://doi.org/10.1097/md.0000000000012111
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or nonprofit sector.
Author information
Authors and Affiliations
Contributions
AMH: Protocol/project development, obstetrics and gynecological surgery, data collection or management, data analysis, manuscript writing/editing. MM: Protocol/project development, data analysis, manuscript writing/editing. AES: Protocol/project development, data collection or management, manuscript writing/editing. AA: Protocol/project development, obstetrics and gynecological surgery, data collection or management, manuscript writing/editing. AK: Protocol/project development, data collection or management, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study declare no conflict of interest and no competing interests with respect to the research, authorship and publication of this article.
Ethical approval
The study protocol was approved by the scientific and ethics committee of Obstetrics and Gynecology department on February 2017.
Informed consent
The participating women were counseled about their condition, the management plan as well as the possible complications, and signed an informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hussein, A.M., Momtaz, M., Elsheikhah, A. et al. The role of ultrasound in prediction of intra-operative blood loss in cases of placenta accreta spectrum disorders. Arch Gynecol Obstet 302, 1143–1150 (2020). https://doi.org/10.1007/s00404-020-05707-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05707-y