Abstract
Purpose
To explore whether the adverse pregnancy outcomes in first frozen embryo transfer (FET) cycles affect live birth and neonatal outcomes in the subsequent pregnancy?
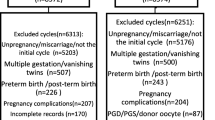
Methods
This was a retrospective study. Women with a history of adverse pregnancy outcomes in first FET cycles started their subsequent embryo transfer cycles. The adverse pregnancy outcomes included biochemical pregnancy, ectopic pregnancy, and first-trimester pregnancy loss. The main outcomes of present study were live birth rate and neonatal outcomes.
Results
Results showed patients with first-trimester pregnancy loss in first FET cycles had a 95 percent greater chance of live birth in subsequent FET cycles (OR 1.95, 95% CI 1.33–2.88). However, the biochemical pregnancy/ectopic pregnancy in initial FET cycles did not affect the chance of live birth in second cycles (biochemical pregnancy: OR 1.21, 95% CI 0.82–1.77; ectopic pregnancy: OR 1.06, 95% CI 0.55–2.05). The neonatal outcomes of singletons were not affected by the number of embryo transfer cycles.
Conclusions
Patients with first-trimester pregnancy loss in first FET cycle had a greater chance of live birth in second FET cycles, but the biochemical pregnancy/ectopic pregnancy in first FET cycles did not significantly affect the live birth in second FET cycles. The three types of adverse pregnancy outcomes in first FET cycles did not affect neonatal outcomes in the second cycles.

Similar content being viewed by others

References
Kushnir VA, Barad DH, Albertini DF, Darmon SK, Gleicher N (2017) Systematic review of worldwide trends in assisted reproductive technology 2004–2013. Reprod Biol Endocrinol: RB&E 15(1):6. https://doi.org/10.1186/s12958-016-0225-2
Niederberger C, Pellicer A, Cohen J, Gardner DK, Palermo GD, O'Neill CL, Chow S, Rosenwaks Z, Cobo A, Swain JE, Schoolcraft WB, Frydman R, Bishop LA, Aharon D, Gordon C, New E, Decherney A, Tan SL, Paulson RJ, Goldfarb JM, Brännström M, Donnez J, Silber S, Dolmans M-M, Simpson JL, Handyside AH, Munné S, Eguizabal C, Montserrat N, Belmonte JCI, Trounson A, Simon C, Tulandi T, Giudice LC, Norman RJ, Hsueh AJ, Sun Y, Laufer N, Kochman R, Eldar-Geva T, Lunenfeld B, Ezcurra D, D'Hooghe T, Fauser BCJM, Tarlatzis BC, Meldrum DR, Casper RF, Fatemi HM, Devroey P, Galliano D, Wikland M, Sigman M, Schoor RA, Goldstein M, Lipshultz LI, Schlegel PN, Hussein A, Oates RD, Brannigan RE, Ross HE, Pennings G, Klock SC, Brown S, Van Steirteghem A, Rebar RW, LaBarbera AR (2018) Forty years of IVF. Fertil Steril 110(2):185–324. https://doi.org/10.1016/j.fertnstert.2018.06.005
Qin J, Liu X, Sheng X, Wang H, Gao S (2016) Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril 105(1):73–85. https://doi.org/10.1016/j.fertnstert.2015.09.007
Yang X, Li Y, Li C, Zhang W (2014) Current overview of pregnancy complications and live-birth outcome of assisted reproductive technology in mainland China. Fertil Steril 101(2):385–391. https://doi.org/10.1016/j.fertnstert.2013.10.017
Stanhiser J, Steiner AZ (2018) Psychosocial aspects of fertility and assisted reproductive technology. Obstet Gyn Clin N Am 45(3):563–574. https://doi.org/10.1016/j.ogc.2018.04.006
Haimovici F, Anderson JL, Bates GW, Racowsky C, Ginsburg ES, Simovici D, Fichorova RN (2018) Stress, anxiety, and depression of both partners in infertile couples are associated with cytokine levels and adverse IVF outcome. Am J Reprod Immunol 79(4):e12832. https://doi.org/10.1111/aji.12832 (New York, N.Y.: 1989)
Wang ET, Kathiresan A, Bresee C, Greene N, Alexander C, Pisarska MD (2017) Abnormal implantation after fresh and frozen in vitro fertilization cycles. Fertil Steril 107(5):1153–1158. https://doi.org/10.1016/j.fertnstert.2017.03.012
Londra L, Moreau C, Strobino D, Garcia J, Zacur H, Zhao Y (2015) Ectopic pregnancy after invitro fertilization: differences between fresh and frozen-thawed cycles. Fertil Steril 104(1):110–118
Hipp H, Crawford S, Kawwass JF, Chang J, Kissin DM, Jamieson DJ (2016) First trimester pregnancy loss after fresh and frozen invitro fertilization cycles. Fertil Steril 105(3):722–728
Santosribeiro S, Tournaye H, Polyzos NP (2016) Trends in ectopic pregnancy rates following assisted reproductive technologies in the UK: a 12-year nationwide analysis including 160 000 pregnancies. Hum Reprod 35(2):474–488
Du T, Chen H, Fu R, Chen Q, Wang Y, Mol BW, Kuang Y, Lyu Q (2017) Comparison of ectopic pregnancy risk among transfers of embryos vitrified on day 3, day 5, and day 6. Fertil Steril 108(1):108–116
Roque M, Valle M, Guimarães F, Sampaio M, Geber S (2015) Freeze-all policy: fresh vs. frozen-thawed embryo transfer. Fertil Steril 103(5):1190–1193
Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X, Cao Y, Yang J, Liu J, Wei D, Weng N (2016) Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. New Engl J Med 375(6):523–533
Roque M, Valle M, Kostolias A, Sampaio M, Geber S (2017) Freeze-all cycle in reproductive medicine: current perspectives. JBRA Assist Reprod 21(1):49–53. https://doi.org/10.5935/1518-0557.20170012
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S (2011) Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril 96(2):344–348. https://doi.org/10.1016/j.fertnstert.2011.05.050
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S (2011) Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfers in high responders. Fertil Steril 96(2):516–518. https://doi.org/10.1016/j.fertnstert.2011.02.059
Zhu Q, Chen Q, Wang L, Lu X, Lyu Q, Wang Y, Kuang Y (2018) Live birth rates in the first complete IVF cycle among 20 687 women using a freeze-all strategy. Hum Reprod. https://doi.org/10.1093/humrep/dey044
Kuang Y, Hong Q, Chen Q, Lyu Q, Ai A, Fu Y, Shoham Z (2014) Luteal-phase ovarian stimulation is feasible for producing competent oocytes in women undergoing in vitro fertilization/intracytoplasmic sperm injection treatment, with optimal pregnancy outcomes in frozen-thawed embryo transfer cycles. Fertil Steril 101(1):105–111. https://doi.org/10.1016/j.fertnstert.2013.09.007
Kuang Y, Chen Q, Hong Q, Lyu Q, Ai A, Fu Y, Shoham Z (2014) Double stimulations during the follicular and luteal phases of poor responders in IVF/ICSI programmes (Shanghai protocol). Reprod Biomed Online 29(6):684–691. https://doi.org/10.1016/j.rbmo.2014.08.009
Chen H, Wang Y, Lyu Q, Ai A, Fu Y, Tian H, Cai R, Hong Q, Chen Q, Shoham Z, Kuang Y (2015) Comparison of live-birth defects after luteal-phase ovarian stimulation vs. conventional ovarian stimulation for in vitro fertilization and vitrified embryo transfer cycles. Fertil Steril 103(5):1194–1201. https://doi.org/10.1016/j.fertnstert.2015.02.020
Cummins JM, Breen TM, Harrison KL, Shaw JM, Wilson LM, Hennessey JF (1986) A formula for scoring human embryo growth rates in in vitro fertilization: its value in predicting pregnancy and in comparison with visual estimates of embryo quality. J In Vitro Fert Embryo Transf 3(5):284–295
Reinblatt SL, Ishai L, Shehata F, Son WY, Tulandi T, Almog B (2011) Effects of ovarian endometrioma on embryo quality. Fertil Steril 95(8):2700–2702. https://doi.org/10.1016/j.fertnstert.2011.03.002
Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y, Mao M, Wang Y, Li Q, Ma S, Ma X, Zhang Y (2014) Birth weight reference percentiles for Chinese. PLoS ONE 9(8):e104779. https://doi.org/10.1371/journal.pone.0104779
Wang YA, Kovacs G, Sullivan EA (2010) Transfer of a selected single blastocyst optimizes the chance of a healthy term baby: a retrospective population based study in Australia 2004–2007. Hum Reprod 25(8):1996–2005. https://doi.org/10.1093/humrep/deq145
Kissin DM, Kulkarni AD, Kushnir VA, Jamieson DJ (2014) Number of embryos transferred after in vitro fertilization and good perinatal outcome. Obstet Gynecol 123(2 PART 1):239–247
Kawwass JF, Badell ML (2018) Maternal and fetal risk associated with assisted reproductive technology. Obstet Gynecol 132(3):763–772. https://doi.org/10.1097/AOG.0000000000002786
Shaw JL, Dey SK, Critchley HO, Horne AW (2010) Current knowledge of the aetiology of human tubal ectopic pregnancy. Hum Reprod Update 16(4):432–444. https://doi.org/10.1093/humupd/dmp057
Krieg SA, Shahine LK, Lathi RB (2016) Environmental exposure to endocrine-disrupting chemicals and miscarriage. Fertil Steril 106(4):941–947
Varner MW, Silver RM, Rowland Hogue CJ, Willinger M, Parker CB, Thorsten VR, Goldenberg RL, Saade GR, Dudley DJ, Coustan D, Stoll B, Bukowski R, Koch MA, Conway D, Pinar H, Reddy UM (2014) Association between stillbirth and illicit drug use and smoking during pregnancy. Obstet Gynecol 123(1):113–125
Law YJ, Zhang N, Venetis CA, Chambers GM, Harris K (2019) The number of oocytes associated with maximum cumulative live birth rates per aspiration depends on female age: a population study of 221 221 treatment cycles. Hum Reprod (Oxford, England) 34(9):1778–1787. https://doi.org/10.1093/humrep/dez100
Quinn MM, Rosen MP, Allen IE, Huddleston HG, Cedars MI, Fujimoto VY (2019) Interpregnancy interval and singleton pregnancy outcomes after frozen embryo transfer. Fertil Steril 111(6):1145–1150. https://doi.org/10.1016/j.fertnstert.2019.02.018
Xu LC, Qiang ZW, Wang L (2002) The timing of marriage in China. Ann Econ Financ 4(2):343–357
Liu Q (2017) China’s leftover women: late marriage among professional women and its consequences. Asian J Women Stud 31(4):471–474
Sneeringer R, Klipstein S, Ryley DA, Alper MM, Reindollar RH (2008) Pregnancy loss in the first in vitro fertilization cycle is not predictive of subsequent delivery in women over 40 years. Fertil Steril 89(2):364–367
Yang R, Yang S, Li R, Chen X, Wang H, Ma C, Liu P, Qiao J (2015) Biochemical pregnancy and spontaneous abortion in first IVF cycles are negative predictors for subsequent cycles: an over 10,000 cases cohort study. Arch Gynecol Obstet 292(2):453–458. https://doi.org/10.1007/s00404-015-3639-8
Wright Bates G Jr, Ginsburg ES (2002) Early pregnancy loss in in vitro fertilization (IVF) is a positive predictor of subsequent IVF success. Fertil Steril 77(2):337–341
Choudhury SR, Knapp LA (2001) Human reproductive failure I: immunological factors. Hum Reprod Update 7(2):113–134. https://doi.org/10.1093/humupd/7.2.113
Choudhury SR, Knapp LA (2001) Human reproductive failure II: immunogenetic and interacting factors. Hum Reprod Update 7(2):135–160. https://doi.org/10.1093/humupd/7.2.135
Troncoso C, Bosch E, Rubio C, Remohí J, Simón C, Pellicer A (2003) The origin of biochemical pregnancies: lessons learned from preimplantation genetic diagnosis. Fertil Steril 79(2):449–450. https://doi.org/10.1016/s0015-0282(02)04670-8
Gaskins AJ, Missmer SA, Rich-Edwards JW, Williams PL, Souter I, Chavarro JE (2018) Demographic, lifestyle, and reproductive risk factors for ectopic pregnancy. Fertil Steril 110(7):1328–1337. https://doi.org/10.1016/j.fertnstert.2018.08.022
Jivraj S, Anstie B, Cheong YC, Fairlie FM, Laird SM, Li TC (2001) Obstetric and neonatal outcome in women with a history of recurrent miscarriage: a cohort study. Hum Reprod 16(1):102–106. https://doi.org/10.1093/humrep/16.1.102
Bhattacharya S, Townend J, Shetty A, Campbell D, Bhattacharya S (2008) Does miscarriage in an initial pregnancy lead to adverse obstetric and perinatal outcomes in the next continuing pregnancy? BJOG 115(13):1623–1629. https://doi.org/10.1111/j.1471-0528.2008.01943.x
Barnhart KT (2014) Are we ready to eliminate the transfer of fresh embryos in IVF? Fertil Steril 102(1):1–2. https://doi.org/10.1016/j.fertnstert.2014.05.024
Evans J, Hannan NJ, Edgell TA, Vollenhoven BJ, Lutjen PJ, Osianlis T, Salamonsen LA, Rombauts LJ (2014) Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update 20(6):808–821. https://doi.org/10.1093/humupd/dmu027
Roque M, Lattes K, Serra S, Solà I, Geber S, Carreras R, Checa MA (2013) Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril 99(1):156–162
Acknowledgements
The authors wish to express their thanks to all clinicians and clinical embryologists in the Department of Assisted Reproduction.
Funding
This work was supported by National Natural Science Foundation of China (Grant Nos. 81903324, 81771533, 81571397 and 81701523).
Author information
Authors and Affiliations
Contributions
YPK and QQZ designed the study. QQZ and JHL drafted the manuscript. JYL and YMR conducted the data acquisition and statistical analysis. YPK revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All participants gave written informed consent for this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J., Lin, J., Yin, M. et al. The live birth and neonatal outcomes in the subsequent pregnancy among patients with adverse pregnancy outcomes in first frozen embryo transfer cycles. Arch Gynecol Obstet 302, 731–740 (2020). https://doi.org/10.1007/s00404-020-05608-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05608-0