Abstract
Purpose
Identify a group with a high risk of postoperative complications after deep bowel endometriosis surgery.
Methods
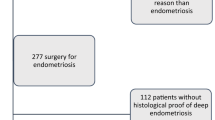
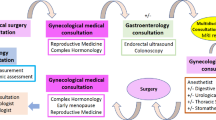
We conducted a retrospective study on patients treated from 2012 to 2018 in two departments of gynecological surgery at the Toulouse University Hospital, France. The postoperative complications were evaluated in relation to the surgical management, associated with or without non-digestive surgical procedures, initial disease and patient's characteristics.
Results
164 patients were included. A postoperative complication occurred in 37.8% (n = 62) of the cases and required a secondary surgery in 18.3% (n = 30) of the cases. In the univariate analysis, the risk of postoperative complications increased significantly in the presence of segmental resection, disease progression, and associated urinary tract procedure or vaginal incision.
In the multivariate analysis, the risk of overall postoperative complications was associated with the surgical management (p = 0.013 and 0.017) and particularly in the presence of segmental resection [Odds Ratio (OR): 20.87; CI 95% (1.96–221.79)]. The risk of rectovaginal fistula increased in the presence of segmental resection [OR: 22.71; CI 95% (2.74–188.01)] as well as in vaginal incision [OR: 19.67; CI 95% (2.43–159.18); p = 0.005].
Conclusion
The risk of overall postoperative complications and rectovaginal fistula in particular increases significantly in the presence of vaginal incision, segmental resection and urinary tract procedures after deep bowel endometriosis surgery.
Similar content being viewed by others
References
de Ziegler D, Borghese B, Chapron C (2010) Endometriosis and infertility: pathophysiology and management. Lancet Lond Engl 376:730–738
Maignien C et al (2017) Prognostic factors for assisted reproductive technology in women with endometriosis-related infertility. Am J Obstet Gynecol 216(280):e1–280.e9
Pluchino N et al (2016) Sexual function in endometriosis patients and their partners: effect of the disease and consequences of treatment. Hum Reprod Update 22:762–774
Nnoaham KE et al (2011) Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 96:366–373.e8
Facchin F et al (2015) Impact of endometriosis on quality of life and mental health: pelvic pain makes the difference. J Psychosom Obstet Gynaecol 36:135–141
Márki G, Bokor A, Rigó J, Rigó A (2017) Physical pain and emotion regulation as the main predictive factors of health-related quality of life in women living with endometriosis. Hum Reprod Oxf Engl 32:1432–1438
Minelli L et al (2009) Laparoscopic colorectal resection for bowel endometriosis: feasibility, complications, and clinical outcome. Arch Surg Chic 144:234–239 (discussion 239)
De Cicco C et al (2011) Bowel resection for deep endometriosis: a systematic review. BJOG Int J Obstet Gynaecol 118:285–291
Coronado C, Franklin RR, Lotze EC, Bailey HR, Valdés CT (1990) Surgical treatment of symptomatic colorectal endometriosis. Fertil Steril 53:411–416
Tran KT, Kuijpers HC, Willemsen WN, Bulten H (1996) Surgical treatment of symptomatic rectosigmoid endometriosis. Eur J Surg Acta Chir 162:139–141
Jerby BL, Kessler H, Falcone T, Milsom JW (1999) Laparoscopic management of colorectal endometriosis. Surg Endosc 13:1125–1128
Remorgida V, Ferrero S, Fulcheri E, Ragni N, Martin DC (2007) Bowel endometriosis: presentation, diagnosis, and treatment. Obstet Gynecol Surv 62:461–470
Bailey HR, Ott MT, Hartendorp P (1994) Aggressive surgical management for advanced colorectal endometriosis. Dis Colon Rectum 37:747–753
Darai E et al (2005) Feasibility and clinical outcome of laparoscopic colorectal resection for endometriosis. Am J Obstet Gynecol 192:394–400
Nyangoh Timoh K et al (2018) Magnetic resonance enterography to assess multifocal and multicentric bowel endometriosis. J Minim Invasive Gynecol 25:697–705
Berlanda N et al (2017) Surgery versus hormonal therapy for deep endometriosis: is it a choice of the physician? Eur J Obstet Gynecol Reprod Biol 209:67–71
Millochau J-C et al (2016) Continuous amenorrhea may be insufficient to stop the progression of colorectal endometriosis. J Minim Invasive Gynecol 23:839–842
Zheng Y et al (2018) Rectovaginal fistula following surgery for deep infiltrating endometriosis: does lesion size matter? J Int Med Res 46:852–864
Abo C et al (2018) Postoperative complications after bowel endometriosis surgery by shaving, disc excision, or segmental resection: a three-arm comparative analysis of 364 consecutive cases. Fertil Steril 109:172–178.e1
Riiskjær M et al (2017) Diagnostic value of serial measurement of c-reactive protein in the detection of a surgical complication after laparoscopic bowel resection for endometriosis. Gynecol Obstet Invest 82:410–416
Oliveira MAP et al (2016) Bowel complications in endometriosis surgery. Best Pract Res Clin Obstet Gynaecol 35:51–62
Vallée A et al (2018) Surgery for deep endometriosis without involvement of digestive or urinary tracts: do not worry the patients! Fertil Steril 109:1079–1085.e1
Working group of ESGE, ESHRE, and WES et al (2020) Recommendations for the surgical treatment of endometriosis. Part 2: deep endometriosis. Hum Reprod Open 2020:hoaa002
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Belghiti J et al (2014) Role of protective defunctioning stoma in colorectal resection for endometriosis. J Minim Invasive Gynecol 21:472–479
Knabben L et al (2015) Urinary tract endometriosis in patients with deep infiltrating endometriosis: prevalence, symptoms, management, and proposal for a new clinical classification. Fertil Steril 103:147–152
Saavalainen L, Heikinheimo O, Tiitinen A, Härkki P (2016) Deep infiltrating endometriosis affecting the urinary tract-surgical treatment and fertility outcomes in 2004–2013. Gynecol Surg 13:435–444
Erdem S et al (2018) Functional outcomes after rectal resection for deep infiltrating pelvic endometriosis: long-term results. Dis Colon Rectum 61:733–742
Hudelist G et al (2018) Pain and fertility outcomes of nerve-sparing, full-thickness disk or segmental bowel resection for deep infiltrating endometriosis—a prospective cohort study. Acta Obstet Gynecol Scand 97:1438–1446
Hudelist G et al (2018) Outcome of sonography-based minimally invasive surgery for deep infiltrating endometriosis of the ureter and urinary bladder—a retrospective cohort study. Acta Obstet Gynecol Scand 97:277–284
Bendifallah S et al (2018) Impact of hospital and surgeon case volume on morbidity in colorectal endometriosis management: a plea to define criteria for expert centers. Surg Endosc 32:2003–2011
Roman H (2017) A national snapshot of the surgical management of deep infiltrating endometriosis of the rectum and colon in France in 2015: a multicenter series of 1135 cases. J Gynecol Obstet Hum Reprod 46:159–165
Kondo W et al (2011) Complications after surgery for deeply infiltrating pelvic endometriosis. BJOG Int J Obstet Gynaecol 118:292–298
Fanfani F et al (2010) Discoid or segmental rectosigmoid resection for deep infiltrating endometriosis: a case-control study. Fertil Steril 94:444–449
Guo S-W (2009) Recurrence of endometriosis and its control. Hum Reprod Update 15:441–461
Weir E, Mustard C, Cohen M, Kung R (2005) Endometriosis: what is the risk of hospital admission, readmission, and major surgical intervention? J Minim Invasive Gynecol 12:486–493
Vignali M et al (2005) Surgical treatment of deep endometriosis and risk of recurrence. J Minim Invasive Gynecol 12:508–513
Fedele L et al (2006) Laparoscopic excision of recurrent endometriomas: long-term outcome and comparison with primary surgery. Fertil Steril 85:694–699
Busacca M et al (2006) Determinants of long-term clinically detected recurrence rates of deep, ovarian, and pelvic endometriosis. Am J Obstet Gynecol 195:426–432
Meuleman C et al (2011) Surgical treatment of deeply infiltrating endometriosis with colorectal involvement. Hum Reprod Update 17:311–326
Roman H et al (2016) Long-term functional outcomes following colorectal resection versus shaving for rectal endometriosis. Am J Obstet Gynecol 215(762):e1–762.e9
Jayot A, Nyangoh Timoh K, Bendifallah S, Ballester M, Darai E (2018) Comparison of laparoscopic discoid resection and segmental resection for colorectal endometriosis using a propensity score matching analysis. J Minim Invasive Gynecol 25:440–446
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Contributions
HG: manuscript writing, data collection, project development, CV: project development, data collection, PL: project development, data collection, AG: data analysis, BA: data collection, project development, PG: data collection, SK: project development, BS: project development, SM: project development, JR: project development, AW: project development, EC: manuscript writing, data collection, project development.
Corresponding author
Ethics declarations
Conflict of interest
The authors hereby declare that there is no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gornes, H., Vaysse, C., Leguevaque, P. et al. Identification of a group with high risk of postoperative complications after deep bowel endometriosis surgery: a retrospective study on 164 patients. Arch Gynecol Obstet 302, 383–391 (2020). https://doi.org/10.1007/s00404-020-05604-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05604-4