Abstract
Purpose
To evaluate the association of sonographic fetal head circumference (HC) with obstetric anal sphincter injury (OASIS) occurrence among primiparous women who underwent vacuum-assisted delivery (VAD).
Methods
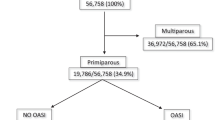
A retrospective study of all primiparous women who delivered at term by VAD between 2011 and 2019 and underwent ultrasound with fetal biometry within 1 week prior to delivery. Women who suffered OASIS were compared to women without OASIS.
Results
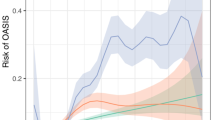
Overall, 74 of 3222 (2.3%) primiparous women suffered an OASIS. As compared with control, women with OASIS were younger (median 28 vs. 30 years, p = 0.001), had higher BMI (median 28.2 vs. 26.9 kg/m2, p = 0.03), and had a longer second stage of labor (median 190 vs. 168 min, p = 0.01). Fetal head circumference was larger in the OASIS group (mean 334 vs. 330 mm, p = 0.03), occiput posterior fetal head position was more prevalent (12 (16%) vs. 232 (7.4%), OR [95% CI]: 2.43 (1.29–4.57), p = 0.004), and the rate of mediolateral episiotomy performed was lower (58 (78.0%) vs. 2777 (88.2%), OR [95% CI]: 0.48 (0.27–0.85), p = 0.01). Multivariate regression modeling identified higher fetal HC (aOR [95% CI] 1.03 (1.001–1.06), p = 0.04) and occiput posterior (aOR [95% CI] 2.5 (1.16–5.71), p = 0.01) as independently positively associated with OASIS. Mediolateral episiotomy and maternal age were independently negatively associated with an OASIS (aOR [95% CI] 0.39 (0.18–0.85), p = 0.01); aOR [95% CI] 0.4 (0.17–0.60), p = 0.001).
Conclusions
Sonographic large fetal HC is associated with OASIS occurrence during VAD. The only modifiable predictor of OASIS detected was mediolateral episiotomy, found to be protective against OASIS.

Similar content being viewed by others
Abbreviations
- OASIS:
-
Obstetric anal sphincter injury
- VAD:
-
Vacuum-assisted delivery
References
Bulletins—Obstetrics CoP (2015) ACOG Practice Bulletin No. 154: operative vaginal delivery. Obstet Gynecol 126:e56–65
Eason E, Labrecque M, Wells G, Feldman P (2000) Preventing perineal trauma during childbirth: a systematic review. Obstet Gynecol 95:464–471
O'Mahony F, Hofmeyr GJ, Menon V (2010) Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005455.pub2
Robinson JN, Norwitz ER, Cohen AP, McElrath TF, Lieberman ES (1999) Episiotomy, operative vaginal delivery, and significant perinatal trauma in nulliparous women. Am J Obstet Gynecol 181:1180–1184
Ramm O, Woo VG, Hung YY, Chen HC, Ritterman Weintraub ML (2018) Risk factors for the development of obstetric anal sphincter injuries in modern obstetric practice. Obstet Gynecol 131:290–296
Nordenstam J, Altman D, Brismar S, Zetterström J (2009) Natural progression of anal incontinence after childbirth. Int Urogynecol J Pelvic Floor Dysfunct 20:1029–1035
Bols EM, Hendriks EJ, Berghmans BC, Baeten CG, Nijhuis JG, de Bie RA (2010) A systematic review of etiological factors for postpartum fecal incontinence. Acta Obstet Gynecol Scand 89:302–314
Abbott D, Atere-Roberts N, Williams A, Oteng-Ntim E, Chappell LC (2010) Obstetric anal sphincter injury. BMJ 341:c3414
Ryman P, Ahlberg M, Ekéus C (2015) Risk factors for anal sphincter tears in vacuum-assisted delivery. Sex Reprod Healthc 6:151–156
Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A (2014) Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol 210(59):e1–6
Waldman R (2019) ACOG Practice Bulletin No. 198: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol 133:185
Gundabattula SR, Surampudi K (2018) Risk factors for obstetric anal sphincter injuries (OASI) at a tertiary centre in south India. Int Urogynecol J 29:391–396
Räisänen S, Vehviläinen-Julkunen K, Cartwright R, Gissler M, Heinonen S (2012) Vacuum-assisted deliveries and the risk of obstetric anal sphincter injuries-a retrospective register-based study in Finland. BJOG 119:1370–1378
Wu JM, Williams KS, Hundley AF, Connolly A, Visco AG (2005) Occiput posterior fetal head position increases the risk of anal sphincter injury in vacuum-assisted deliveries. Am J Obstet Gynecol 193:525–528 (discussion 28–29)
Levin G, Rottenstreich A, Cahan T et al (2020) Does birthweight have a role in the effect of episiotomy on anal sphincter injury? Arch Gynecol Obstet 301:171–177
Gommesen D, Nohr EA, Drue HC, Qvist N, Rasch V (2019) Obstetric perineal tears: risk factors, wound infection and dehiscence: a prospective cohort study. Arch Gynecol Obstet 300:67–77
Kabiri D, Lipschuetz M, Cohen SM et al (2019) Vacuum extraction failure is associated with a large head circumference. J Matern Fetal Neonatal Med 32:3325–3330
Lipschuetz M, Cohen SM, Ein-Mor E et al (2015) A large head circumference is more strongly associated with unplanned cesarean or instrumental delivery and neonatal complications than high birthweight. Am J Obstet Gynecol 213:833.e1–33.e12
Baghestan E, Irgens LM, Børdahl PE, Rasmussen S (2010) Trends in risk factors for obstetric anal sphincter injuries in Norway. Obstet Gynecol 116:25–34
Selmer-Olsen T, Nohr EA, Tappert C, Eggebø TM (2019) Incidence and risk factors for obstetric anal sphincter ruptures, OASIS, following the introduction of preventive interventions. A retrospective cohort study from a Norwegian hospital 2012–2017. Sex Reprod Healthc 22:100460
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 144:768–773
Salomon LJ, Alfirevic Z, Da Silva CF et al (2019) ISUOG Practice Guidelines: ultrasound assessment of fetal biometry and growth. Ultrasound Obstet Gynecol 53:715–723
Hadlock FP, Harrist RB, Carpenter RJ, Deter RL, Park SK (1984) Sonographic estimation of fetal weight. The value of femur length in addition to head and abdomen measurements. Radiology 150:535–540
Lipschuetz M, Cohen SM, Israel A et al (2018) Sonographic large fetal head circumference and risk of cesarean delivery. Am J Obstet Gynecol 218:339.e1–39.e7
Valsky DV, Lipschuetz M, Bord A et al (2009) Fetal head circumference and length of second stage of labor are risk factors for levator ani muscle injury, diagnosed by 3-dimensional transperineal ultrasound in primiparous women. Am J Obstet Gynecol 201(91):e1–7
Kudish B, Sokol RJ, Kruger M (2008) Trends in major modifiable risk factors for severe perineal trauma, 1996–2006. Int J Gynaecol Obstet 102:165–170
Drusany Starič K, Bukovec P, Jakopič K, Zdravevski E, Trajkovik V, Lukanović A (2017) Can we predict obstetric anal sphincter injury? Eur J Obstet Gynecol Reprod Biol 210:196–200
Bulletins—Obstetrics ACoOaGCoP (2016) Practice Bulletin No. 173: Fetal Macrosomia. Obstet Gynecol 128:e195–e209
Levin G, Meyer R, Yagel S, David M, Yinon Y, Rottenstreich A (2020) Which way is better to deliver the very heavy baby: mode of delivery, maternal and neonatal outcome. Arch Gynecol Obstet 301(4):941–948
Melamed N, Yogev Y, Meizner I, Mashiach R, Ben-Haroush A (2010) Sonographic prediction of fetal macrosomia: the consequences of false diagnosis. J Ultrasound Med 29:225–230
Melamed N, Yogev Y, Danon D, Mashiach R, Meizner I, Ben-Haroush A (2011) Sonographic estimation of fetal head circumference: how accurate are we? Ultrasound Obstet Gynecol 37:65–71
Pergialiotis V, Vlachos D, Protopapas A, Pappa K, Vlachos G (2014) Risk factors for severe perineal lacerations during childbirth. Int J Gynaecol Obstet 125:6–14
Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD (2015) Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol 125:927–937
Lund NS, Persson LK, Jangö H, Gommesen D, Westergaard HB (2016) Episiotomy in vacuum-assisted delivery affects the risk of obstetric anal sphincter injury: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 207:193–199
Deane RP (2019) Operative vaginal delivery and pelvic floor complications. Best Pract Res Clin Obstet Gynaecol 56:81–92
Franchi M, Parissone F, Lazzari C et al (2020) Selective use of episiotomy: what is the impact on perineal trauma? Results from a retrospective cohort study. Arch Gynecol Obstet 301:427–435
Levin G, Rottenstreich A (2019) Operative delivery in nuliiparous: deserves an episiotomy. Arch Gynecol Obstet 300:1473–1474
Richter HE, Brumfield CG, Cliver SP, Burgio KL, Neely CL, Varner RE (2002) Risk factors associated with anal sphincter tear: a comparison of primiparous patients, vaginal births after cesarean deliveries, and patients with previous vaginal delivery. Am J Obstet Gynecol 187:1194–1198
Revicky V, Nirmal D, Mukhopadhyay S, Morris EP, Nieto JJ (2010) Could a mediolateral episiotomy prevent obstetric anal sphincter injury? Eur J Obstet Gynecol Reprod Biol 150:142–146
Gerdin E, Sverrisdottir G, Badi A, Carlsson B, Graf W (2007) The role of maternal age and episiotomy in the risk of anal sphincter tears during childbirth. Aust N Z J Obstet Gynaecol 47:286–290
Loewenberg-Weisband Y, Grisaru-Granovsky S, Ioscovich A, Samueloff A, Calderon-Margalit R (2014) Epidural analgesia and severe perineal tears: a literature review and large cohort study. J Matern Fetal Neonatal Med 27:1864–1869
Funding
No external funding was used in this conduct of this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript. GL, RM and AR reviewed the literature and wrote the paper. MS, MA, ER and YY performed the procedures and collected the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required and was waived by the institutional review board approval. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meyer, R., Rottenstreich, A., Shapira, M. et al. The role of fetal head circumference in the formation of obstetric anal sphincter injuries following vacuum deliveries among primiparous women. Arch Gynecol Obstet 301, 1423–1429 (2020). https://doi.org/10.1007/s00404-020-05558-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05558-7