Abstract
Objective
Data regarding the effect of post-partum bilateral tubal ligation (BTL) on future risk for ovarian cancer (OC) is lacking. In the current study, we aimed to evaluate the effect of BTL during cesarean delivery (CD) on the long-term risk for OC.
Study design
A population-based cohort analysis of women above the age of 35 that underwent CD in their last delivery, comparing the long-term risk for OC between patients that had a Pomeroy excisional BTL and those that did not. OC diagnosis was pre-defined based on ICD-9 codes. Procedures occurred between the years 1991–2017. Kaplan–Meier survival curve was used to compare the cumulative incidence of OC over time and Cox proportional hazards model was constructed to control for confounders.
Results
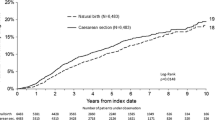
During the study period 13,124 women met the inclusion criteria; 9438 (71.9%) of which had only CD and 3686 (28.1%) underwent CD with BTL. Despite the significantly higher incidence of maternal factors that might increase the long-term risk for OC in the BTL group (advanced maternal age, obesity, hypertensive diseases during pregnancy and diabetes mellitus), the cumulative incidence of OC cases was not significantly different between the two groups (Log-rank test p = 0.199). Likewise, when performing a Cox regression model controlling for maternal age, obesity, hypertensive diseases and diabetes, OC risk was not significantly different between the groups (adjusted HR 2.36, 95% CI 0.73–7.62; p = 0.149).
Conclusion
Despite an increased incidence of known risk factors for OC, patients that underwent BTL during CD did not have increased long-term risk for OC.

Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Maringe C, Walters S, Butler J, Coleman MP, Hacker N, Hanna L et al (2012) Stage at diagnosis and ovarian cancer survival: evidence from the International Cancer Benchmarking Partnership. Gynecol Oncol 127(1):75–82
Cannistra SA (2004) Cancer of the ovary. N Engl J Med 351(24):2519–2529
Buys SS, Partridge E, Black A, Johnson CC, Lamerato L, Isaacs C et al (2011) Effect of screening on ovarian cancer mortality: the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Randomized Controlled Trial. JAMA 305(22):2295–2303
Jacobs IJ, Menon U, Ryan A, Gentry-Maharaj A, Burnell M, Kalsi JK et al (2016) Ovarian cancer screening and mortality in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a randomised controlled trial. Lancet 387(10022):945–956
Reid BM, Permuth JB, Sellers TA (2017) Epidemiology of ovarian cancer: a review. Cancer Biol Med 14(1):9–32
Charach R, Sheiner E, Beharier O, Sergienko R, Kessous R (2018) Recurrent pregnancy loss and future risk of female malignancies. Arch Gynecol Obstet 298(4):781–787
Fuchs O, Sheiner E, Meirovitz M, Davidson E, Sergienko R, Kessous R (2017) The association between a history of gestational diabetes mellitus and future risk for female malignancies. Arch Gynecol Obstet 295(3):731–736
Kessous R, Davidson E, Meirovitz M, Sergienko R, Sheiner E (2017) Prepregnancy obesity: a risk factor for future development of ovarian and breast cancer. Eur J Cancer Prev 26(2):151–155
Kurman RJ (2013) Origin and molecular pathogenesis of ovarian high-grade serous carcinoma. Ann Oncol 24(Suppl 10):16–21
Kurman RJ, Vang R, Junge J, Hannibal CG, Kjaer SK, Shih IM (2011) Papillary tubal hyperplasia: the putative precursor of ovarian atypical proliferative (borderline) serous tumors, noninvasive implants, and endosalpingiosis. Am J Surg Pathol 35(11):1605–1614
Jarboe EA, Folkins AK, Drapkin R, Ince TA, Agoston ES, Crum CP (2009) Tubal and ovarian pathways to pelvic epithelial cancer: a pathological perspective. Histopathology 55(5):619
Yoon SH, Kim SN, Shim SH, Kang SB, Lee SJ (2016) Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: a meta-analysis. Eur J Cancer 55:38–46
Cramer DW, Xu H (1995) Epidemiologic evidence for uterine growth factors in the pathogenesis of ovarian cancer. Ann Epidemiol 5(4):310–314
Pinheiro SP, Hankinson SE, Tworoger SS, Rosner BA, McKolanis JR, Finn OJ et al (2010) Anti-MUC1 antibodies and ovarian cancer risk: prospective data from the Nurses' Health Studies. Cancer Epidemiol Biomark Prev 19(6):1595–1601
Martin JA, Hamilton BE, Osterman MJK (2017) Births in the United States, 2016. NCHS Data Brief 287:1–8
Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR (2016) The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS One 11(2):e0148343
Garcia G, Richardson DM, Gonzales KL, Cuevas AG (2015) Trends and disparities in postpartum sterilization after cesarean section, 2000 through 2008. Womens Health Issues 25(6):634–640
Chan LM, Westhoff CL (2010) Tubal sterilization trends in the United States. Fertil Steril 94(1):1–6
Lawrie TA, Kulier R, Nardin JM (2016) Techniques for the interruption of tubal patency for female sterilisation. Cochrane Database Syst Rev 8:CD003034
Yang M, Du Y, Hu Y (2019) Complete salpingectomy versus tubal ligation during cesarean section: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1690446
Rice MS, Hankinson SE, Tworoger SS (2014) Tubal ligation, hysterectomy, unilateral oophorectomy, and risk of ovarian cancer in the Nurses' Health Studies. Fertil Steril 102(1):192–8.e3
Lessard-Anderson CR, Handlogten KS, Molitor RJ, Dowdy SC, Cliby WA, Weaver AL et al (2014) Effect of tubal sterilization technique on risk of serous epithelial ovarian and primary peritoneal carcinoma. Gynecol Oncol 135(3):423–427
Madsen C, Baandrup L, Dehlendorff C, Kjaer SK (2015) Tubal ligation and salpingectomy and the risk of epithelial ovarian cancer and borderline ovarian tumors: a nationwide case-control study. Acta Obstet Gynecol Scand 94(1):86–94
Cibula D, Widschwendter M, Májek O, Dusek L (2011) Tubal ligation and the risk of ovarian cancer: review and meta-analysis. Hum Reprod Update 17(1):55–67
Rice MS, Murphy MA, Vitonis AF, Cramer DW, Titus LJ, Tworoger SS et al (2013) Tubal ligation, hysterectomy and epithelial ovarian cancer in the New England Case–Control Study. Int J Cancer 133(10):2415–2421
Ely LK, Truong M (2017) The role of opportunistic bilateral salpingectomy vs tubal occlusion or ligation for ovarian cancer prophylaxis. J Minim Invasive Gynecol 24(3):371–378
Funding
No funding.
Author information
Authors and Affiliations
Contributions
RK: project development, data management, manuscript writing. RS: data management, data analysis, manuscript editing. ES: project development, data management, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Author R.K declares that he has no conflict of interest. Author S.R declares that he has no conflict of interest. Author S.E declares that he has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Dig | ICD code | Diagnosis |
|---|---|---|
Ovary | ||
7300 | V1043 | Personal history of malignant neoplasm of ovary |
21,899 | 183 | Malignant neoplasm of ovary and other uterine adnexa |
21,900 | 1830 | Malignant neoplasm of ovary |
21,901 | 1832 | Malignant neoplasm of ovary |
21,905 | 1838 | Malignant neoplasm of other specified sites of uterine adnexa |
21,906 | 1839 | Malignant neoplasm of uterine adnexa, unspecified |
21,759 | 1589 | Malignant neoplasm of peritoneum, unspecified |
Rights and permissions
About this article
Cite this article
Kessous, R., Sergienko, R. & Sheiner, E. Tubal ligation during cesarean delivery and future risk for ovarian cancer: a population-based cohort study. Arch Gynecol Obstet 301, 1473–1477 (2020). https://doi.org/10.1007/s00404-020-05547-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05547-w