Abstract
Objective
In an attempt to shed new light on the pathogenesis of fetal growth restriction (FGR), we aimed to study pregnancy characteristics, neonatal outcomes, and placental histopathological lesions of FGR pregnancies in two different subgroups: when developed after appropriate for gestational age (AGA) pregnancy and when developed after previous pregnancy with FGR.
Study design
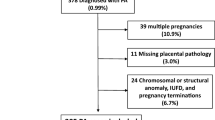
Pregnancy and placental reports of all singleton pregnancies complicated by FGR (defined as actual birthweight below the 10th percentile according to local birthweight nomograms) between 2008 and 2018 were reviewed. Included were only cases with previous delivery. Maternal background, neonatal outcomes, and placental histopathology were compared between FGR that occurred after FGR (recurrent FGR group) and FGR that occurred after an AGA pregnancy (FGR after AGA group). Placental lesions were classified according to the current “Amsterdam” criteria. Continuous variables were compared using the Student’s t test or the Mann–Whitney test as appropriate. Categorical variables were compared using Chi-square or Fisher’s exact test as appropriate.
Results
A total of 334 FGR cases with a previous delivery were included in the study. Of them, 111 cases constituted the recurrent FGR group and 223 constituted the FGR after AGA group. The recurrent FGR group was characterized by higher rates of maternal diabetes during pregnancy and hypertensive diseases (9% versus 2.7%, p = 0.01 and 19.8% versus 11.6%, p = 0.04). The FGR after AGA group was characterized by a higher rate of fetal vascular malperfusion (FVM) lesions (29.6% versus 18.0%, p = 0.02), and by lower mean birthweight (1842 ± 424.9 versus 1977.4 ± 412.2, p = 0.005), as compared to the recurrent FGR group.
Conclusion
Recurrent FGR was associated with maternal background morbidities during pregnancy which represents a chronic repeated insult, while “new” FGR cases (those followed an AGA pregnancy) were characterized by a higher rate of FVM lesions and lower birthweight which probably represent an “accident” in placentation. These findings may suggest that different mechanisms of placental dysfunction exist in the two subgroups of FGR.

Similar content being viewed by others
References
Brosens I, Pijnenborg R, Vercruysse L, Romero R (2011) The “great Obstetrical Syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol 204:193–201. https://doi.org/10.1016/j.ajog.2010.08.009
Kovo M, Schreiber L, Bar J (2013) Placental vascular pathology as a mechanism of disease in pregnancy complications. Thromb Res 131(Suppl):S18–21. https://doi.org/10.1016/S0049-38481370013-6
Ness RB, Sibai BM (2006) Shared and disparate components of the pathophysiologies of fetal growth restriction and preeclampsia. Am J Obstet Gynecol 195:40–49. https://doi.org/10.1016/j.ajog.2005.07.049
Gerretsen G, Huisjes HJ, Elema JD (1981) Morphological changes of the spiral arteries in the placental bed in relation to pre-eclampsia and fetal growth retardation. Br J Obstet Gynaecol 88:876–881
Redline RW, Heller D, Keating S, Kingdom J (2005) Placental diagnostic criteria and clinical correlation a workshop report. Placenta 26:S114–S117. https://doi.org/10.1016/j.placenta2005.02.009
Khong TY, Mooney EE, Ariel I, Balmus NCM, Boyd TK, Brundler M-A, Derricott H, Evans MJ, Faye-Petersen OM, Gillan JE, Heazell AEP, Heller DS, Jacques SM, Keating S, Kelehan P, Maes A, McKay EM, Morgan TK, Nikkels PGJ, Parks WT, Redline RW, Scheimberg I, Schoots MH, Sebire NJ, Timmer A, Turowski G, van der Voorn JP, van Lijnschoten I, Gordijn SJ (2016) Sampling and definitions of placental lesions: amsterdam placental workshop group consensus statement. Arch Pathol Lab Med 140:698–713. https://doi.org/10.5858/arpa.2015-0225-CC
Sharma D, Shastri S, Sharma P (2016) Intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr 10:67–83. https://doi.org/10.4137/CMPed.S40070
Tyson RW, Staat BC (2008) The intrauterine growth-restricted fetus and placenta evaluation. Semin Perinatol 32:166–171. https://doi.org/10.1053/j.semperi.2008.02.005
Vedmedovska N, Rezeberga D, Teibe U, Melderis I, Donders GGG (2011) Placental pathology in fetal growth restriction. Eur J Obstet Gynecol Reprod Biol 155:36–40. https://doi.org/10.1016/j.ejogrb.2010.11.017
Levy M, Mizrachi Y, Leytes S, Weiner E, Bar J, Schreiber L, Kovo M (2018) Can placental histopathology lesions predict recurrence of small for gestational age neonates? Reprod Sci 25:1485–1491. https://doi.org/10.1177/1933719117749757
Levy M, Kovo M, Schreiber L, Kleiner I, Grinstein E, Koren L, Barda G, Bar J, Weiner E (2019) Pregnancy outcomes in correlation with placental histopathology in subsequent pregnancies complicated by fetal growth restriction. Placenta 80:36–41. https://doi.org/10.1016/j.placenta.2019.04.001
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon E (2001) Birth weight standards in the live-born population. Israel Med Assoc J 311:314
Hypertension in pregnancy (2013) Report of the American college of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol 122:1122–1131. https://doi.org/10.1097/01.AOG.0000437382.03963.88
Roberge S, Nicolaides K et al (2016) The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis. Am J Obs Gynecol. 15:30783–30789. https://doi.org/10.1016/j.ajog.2016.09.076
ACOG Practice Bulletin No (2013) 138: Inherited thrombophilias in pregnancy. Obstet Gynecol 122:706–717. https://doi.org/10.1097/01.AOG.0000433981.36184.4e
ACOG Practice Bulletin No (2011) 118: Antiphospholipid syndrome. Obstet Gynecol 117:192–199. https://doi.org/10.1097/AOG.0b013e31820a61f9
Redline RW (2015) Classification of placental lesions. Am J Obstet Gynecol 213:S21–S28. https://doi.org/10.1016/j.ajog.2015.05.056
Weiner E, Mizrachi Y, Grinstein E, Feldstein O, Rymer-Haskel N, Juravel E, Schreiber L, Bar J, Kovo M (2016) The role of placental histopathological lesions in predicting recurrence of preeclampsia. Prenat Diagn 36:953–960. https://doi.org/10.1002/pd.4918
Pinar H, Sung CJ, Oyer CE, Singer DB (1996) Reference values for singleton and twin placental weights. Pediatr Pathol Lab Med J Soc Pediatr Pathol Affil with Int Paediatr Pathol Assoc 16:901–907
Fox GE, Van Wesep R, Resau JH, Sun CC (1991) The effect of immersion formaldehyde fixation on human placental weight. Arch Pathol Lab Med 115:726–728
Strong THJ, Jarles DL, Vega JS, Feldman DB (1994) The umbilical coiling index. Am J Obstet Gynecol 170:29–32
Gaudineau A (2013) Prevalence, risk factors, maternal and fetal morbidity and mortality of intrauterine growth restriction and small-for-gestational age. J Gynecol Obstet Biol Reprod (Paris) 42:895–910. https://doi.org/10.1016/j.jgyn.2013.09.013
Vayssiere C, Sentilhes L, Ego A, Bernard C, Cambourieu D, Flamant C, Gascoin G, Gaudineau A, Grange G, Houfflin-Debarge V, Langer B, Malan V, Marcorelles P, Nizard J, Perrotin F, Salomon L, Senat M-V, Serry A, Tessier V, Truffert P, Tsatsaris V, Arnaud C, Carbonne B (2015) Fetal growth restriction and intra-uterine growth restriction: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol 193:10–18. https://doi.org/10.1016/j.ejogrb.2015.06.021
Hinkle SN, Albert PS, Mendola P, Sjaarda LA, Boghossian NS, Yeung E, Laughon SK (2014) Differences in risk factors for incident and recurrent small-for-gestational-age birthweight: a hospital based cohort study. BJOG discussion. https://doi.org/10.1111/1471-0528.12628
Hooijschuur MCE, Ghossein-Doha C, Kroon AA, de Leeuw PW, Zandbergen AAM, van Kuijk SMJ, Spaanderman MEA (2018) Metabolic Syndrome and Preeclampsia. Ultrasound Obstet Gynecol 54:64–71. https://doi.org/10.1002/uog.20126
Stekkinger E, Scholten RR, Heidema WM, Spaanderman MEA (2015) Recurrent pre-eclampsia in women with metabolic syndrome and low plasma volume: a retrospective cohort study. BJOG 122:1773–1780. https://doi.org/10.1111/1471-0528.13737
Kalafat E, Thilaganathan B (2017) Cardiovascular origins of preeclampsia. Curr Opin Obstet Gynecol 29:383–389. https://doi.org/10.1097/GCO.0000000000000419
Burton GJ, Jauniaux E (2018) Pathophysiology of placental-derived fetal growth restriction. Am J Obstet Gynecol 218:S745–S761. https://doi.org/10.1016/j.ajog.2017.11.577
Boulanger H, Drouin D, Largilliere C, Lefevre G (2019) Intrauterine growth restriction, soluble fms-like tyrosine kinase-1 to placental growth factor ratio increase and preeclampsia. J Gynecol Obstet Hum Reprod 48:695–697. https://doi.org/10.1016/j.jogoh.2019.05.007
Yogev Y, Visser GHA (2009) Obesity, gestational diabetes and pregnancy outcome. Semin Fetal Neonatal Med 14:77–84. https://doi.org/10.1016/j.siny.2008.09.002
Ornoy A (2011) Prenatal origin of obesity and their complications: Gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia. Reprod Toxicol 32:205–212. https://doi.org/10.1016/j.reprotox.2011.05.002
Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, Forest J-C, Giguere Y (2010) Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol 116:402–414. https://doi.org/10.1097/AOG.0b013e3181e9322a
Weiner E, Schreiber L, Grinstein E, Feldstein O, Rymer-Haskel N, Bar J, Kovo M (2016) The placental component and obstetric outcome in severe preeclampsia with and without HELLP syndrome. Placenta 47:99–104. https://doi.org/10.1016/j.placenta.2016.09.012
Redline RW, Ravishankar S (2018) Fetal vascular malperfusion, an update. APMIS 126:561–569. https://doi.org/10.1111/apm.12849
Heider A (2017) Fetal vascular malperfusion. Arch Pathol Lab Med 141:1484–1489. https://doi.org/10.5858/arpa.2017-0212-RA
Chisholm KM, Heerema-McKenney A (2015) Fetal thrombotic vasculopathy: significance in liveborn children using proposed society for pediatric pathology diagnostic criteria. Am J Surg Pathol 39:274–280. https://doi.org/10.1097/PAS.0000000000000334.
Author information
Authors and Affiliations
Contributions
M L: project development, data collection, manuscript writing, D A: data collection, M K: data analysis, L S: placental pathology analysis, E V: data analysis, L K: data collection, J B: manuscript editing, E W: project development, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
There is not any financial relationship with any organization or any conflict of interest to report.
Informed consent
Because the retrospective nature of the study, informed consent was not required in accordance to a specific permission by the local ethics committee decision.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Levy, M., Alberti, D., Kovo, M. et al. Placental pathology in pregnancies complicated by fetal growth restriction: recurrence vs. new onset. Arch Gynecol Obstet 301, 1397–1404 (2020). https://doi.org/10.1007/s00404-020-05546-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05546-x