Abstract
Background
Anti-Müllerian hormone (AMH) used to establish patient profiles and predict ovarian response to stimulation, its role in assisted reproductive technology techniques is crucial.
Purpose
To evaluate the evidence from published RCTs about the efficacy and safety of AMH-based ovarian stimulation versus conventional ovarian stimulation.
Method
Search strategy: electronic databases were searched using the following MeSH terms (Anti-Müllerian hormone OR AMH) AND (IVF OR ICSI) and (tailored OR based). Selection criteria: only RCTs were included. Four studies were included in the quantitative synthesis. Data collection and analysis: the extracted data were entered into RevMan software, the relative risk (RR) and 95% confidence interval (CI) were used for data analysis.
Results
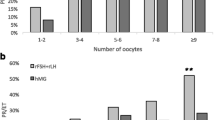
Primary outcomes: ongoing pregnancy: test for overall effect was in favor of AMH-based group, but there was no statistically significant difference [RR = 0.95, 95% CI (0.84–1.08), P = 0.44]. Severe ovarian hyperstimulation syndrome (OHSS) test or overall effect was in favor of AMH-based group, but there was still no statistically significant difference [RR = 0.68, 95% CI (0.43–1.06), P = 0.09]. Secondary outcomes were dose of rFSH, the number of oocytes retrieved, fertilized oocytes, embryos (day 3), blastocysts (day 5), and duration of stimulation. Only the dose of rFSH and duration of stimulation were in the favor of AMH-based group, with statistically significant difference. The other four secondary outcomes were in the favor of the conventional group but with no statistically significant difference.
Conclusion
AMH-based stimulation has the same results of pregnancy rate and risk of OHSS and can reduce the dose of rFSH and duration of stimulation.











Similar content being viewed by others
References
Victoria M, Labrosse J, Krief F, Cedrin-Durnerin I, Comtet M, Grynberg M (2019) Anti Mullerian hormone: more than a biomarker of female reproductive function. J Gynecol Obstet Hum Repro 48(1):19–24. https://doi.org/10.1016/j.jogoh.2018.10.015
Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, Griesinger G, Kelsey TW, La Marca A, Lambalk C, Mason H, Nelson SM, Visser JA, Wallace WH, Anderson RA (2014) The physiology and clinical utility of anti-Mullerian hormone in women. Hum Repro Update 20(3):370–385. https://doi.org/10.1093/humupd/dmt062
Broer SL, Mol BW, Hendriks D, Broekmans FJ (2009) The role of antiMullerian hormone in prediction of outcome after IVF: comparison with the antral follicle count. Fertil Steril 91(3):705–714. https://doi.org/10.1016/j.fertnstert.2007.12.013
Nelson SM, Klein BM, Arce JC (2015) Comparison of antiMullerian hormone levels and antral follicle count as predictor of ovarian response to controlled ovarian stimulation in good-prognosis patients at individual fertility clinics in two multicenter trials. Fertil Steril 103(4):923–930. https://doi.org/10.1016/j.fertnstert.2014.12.114
Fleming R, Seifer DB, Frattarelli JL, Ruman J (2015) Assessing ovarian response: antral follicle count versus anti-Mullerian hormone. Repro Biomed Online 31(4):486–496. https://doi.org/10.1016/j.rbmo.2015.06.015
Magnusson A, Kallen K, Thurin-Kjellberg A, Bergh C (2018) The number of oocytes retrieved during IVF: a balance between efficacy and safety. Hum Reprod 33(1):58–64. https://doi.org/10.1093/humrep/dex334
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G Cochrane Statistical Methods G (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Lan VT, Linh NK, Tuong HM, Wong PC, Howles CM (2013) Anti-Mullerian hormone versus antral follicle count for defining the starting dose of FSH. Repro Biomed Online 27(4):390–399. https://doi.org/10.1016/j.rbmo.2013.07.008
Nyboe Andersen A, Nelson SM, Fauser BC, Garcia-Velasco JA, Klein BM, Arce JC (2017) Individualized versus conventional ovarian stimulation for in vitro fertilization: a multicenter, randomized, controlled, assessor-blinded, phase 3 noninferiority trial. Fertil Steril 107(2):387–396. https://doi.org/10.1016/j.fertnstert.2016.10.033
Thomas S, Acharya M, Muthukumar K, Chandy A, Kamath MS, Aleyamma TK (2018) Effectiveness of anti-Mullerian hormone-tailored protocol compared to conventional protocol in women undergoing in vitro fertilization: a randomized controlled trial. J Hum Reprod Sci 11(1):24–28. https://doi.org/10.4103/jhrs.JHRS_55_17
Friis Petersen J, Lokkegaard E, Andersen LF, Torp K, Egeberg A, Hedegaard L, Nysom D, Nyboe Andersen A (2019) A randomized controlled trial of AMH-based individualized FSH dosing in a GnRH antagonist protocol for IVF. Hum Reprod Open. 1:hoz003. https://doi.org/10.1093/hropen/hoz003
Broer SL, van Disseldorp J, Broeze KA, Dolleman M, Opmeer BC, Bossuyt P, Eijkemans MJ, Mol BW, Broekmans FJ (2013) Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update 19(1):26–36. https://doi.org/10.1093/humupd/dms041
Liao CC, Lee RK, Lin SY, Lin MH, Hwu YM (2016) Outcomes of anti-Mullerian hormone-tailored ovarian stimulation protocols in in vitro fertilization/intracytoplasmic sperm injection cycles in women of advanced age. Taiwan J Obstet Gynecol 55(2):239–243. https://doi.org/10.1016/j.tjog.2015.03.008
Hehenkamp WJ, Looman CW, Themmen AP, de Jong FH, Te Velde ER, Broekmans FJ (2006) Anti-Mullerian hormone levels in the spontaneous menstrual cycle do not show substantial fluctuation. J Clin Endocrinol Metab 91(10):4057–4063. https://doi.org/10.1210/jc.2006-0331
La Marca A, Stabile G, Artenisio AC, Volpe A (2006) Serum anti-Mullerian hormone throughout the human menstrual cycle. Hum Reprod 21(12):3103–3107. https://doi.org/10.1093/humrep/del291
Tsepelidis S, Devreker F, Demeestere I, Flahaut A, Gervy C, Englert Y (2007) Stable serum levels of anti-Mullerian hormone during the menstrual cycle: a prospective study in normo-ovulatory women. Hum Reprod 22(7):1837–1840. https://doi.org/10.1093/humrep/dem101
Lambalk CB, Banga FR, Huirne JA, Toftager M, Pinborg A, Homburg R, van der Veen F, van Wely M (2017) GnRH antagonist versus long agonist protocols in IVF: a systematic review and meta-analysis accounting for patient type. Human Reprod Update 23(5):560–579. https://doi.org/10.1093/humupd/dmx017
Maheshwari A, Pandey S, Amalraj Raja E, Shetty A, Hamilton M, Bhattacharya S (2018) Is frozen embryo transfer better for mothers and babies? Can cumulative meta-analysis provide a definitive answer? Hum Reprod Update 24(1):35–58. https://doi.org/10.1093/humupd/dmx031
Barbosa CP, Cordts EB, Costa AC, de Oliveira R, de Mendonca MA, Christofolini DM, Bianco B (2014) Low dose of rFSH (100 IU) in controlled ovarian hyperstimulation response: a pilot study. J Ovar Res 7:11. https://doi.org/10.1186/1757-2215-7-11
Practice Committee of the American Society for Reproductive Medicine (2016) Electronic address Aao, Practice Committee of the American Society for reproductive M: prevention and treatment of moderate and severe ovarian hyperstimulation syndrome: a guideline. Fertil Steril 106(7):1634–1647. https://doi.org/10.1016/j.fertnstert.2016.08.048
Carbillon L, Gronier H, Cedrin-Durnerin I, Pharisien I, Nguyen MT, Valensi P, Cosson E (2017) The impact of ovulation induction and ovarian stimulation on the risk of pregnancy-induced hypertension and on neonatal outcomes: a case/control study. Eur J Obstet Gynecol Reprod Biol 217:137–143. https://doi.org/10.1016/j.ejogrb.2017.08.032
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by LC, YL, JL and FW. The first draft of the manuscript was written by LC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cui, L., Lin, Y., Lin, J. et al. AMH-based ovarian stimulation versus conventional ovarian stimulation for IVF/ICSI: a systematic review and meta-analysis. Arch Gynecol Obstet 301, 913–922 (2020). https://doi.org/10.1007/s00404-020-05498-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05498-2