Abstract
Purpose
Malignancies of the vagina are rare, but colposcopy-directed biopsies play a major role in detecting vaginal intraepithelial lesions. Data of accuracy in detecting neoplasia of the vagina are very rare compared to accuracy in detecting cervical neoplasia. The aim of this study was to evaluate the accuracy of colposcopy-directed biopsy in comparison with clinical findings of the examiner.
Methods
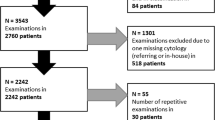
The accuracy of colposcopy-directed biopsy was compared with the clinical finding in relation to the patient’s age and the examiner’s level of training. This was done in combination with PAP-smear, HPV-test results, and the history of other malignancies of the lower genital tract. The data were collected between January 2014 and February 2018 at the certified Dysplasia Unit of the University Hospital Erlangen.
Results
In total, 253 biopsies from 253 women from the vagina were obtained. The overall accuracy of biopsy in comparison with clinical finding was 52.17% for all entities—benign lesions, low-grade squamous intraepithelial lesions (LSILs), high-grade squamous intraepithelial lesions (HSILs), and vaginal carcinoma. The accuracy for detecting HSIL was 82.46% (47/57), with an underdiagnosis rate of 15.79% and an overdiagnosis rate of 1.79%.
Conclusion
With a sensitivity of over 80%, colposcopy-directed biopsy plays an important role in detecting vaginal–HSIL. A highly experienced practitioner is increasing the sensitivity in detecting vaginal–HSIL. Careful examination is required in women with a history of HSIL of the lower genital tract or with simultaneous neoplasia because they are of greater risk of developing vaginal malignancies. The combination of careful clinical work up, PAP-smear, HPV-testing, and colposcopy-guided biopsy is crucial in detecting vaginal–HSIL.





Similar content being viewed by others
References
Shrivastava SB et al (2015) Management of vaginal cancer. Rev Recent Clin Trials 10(4):289–297
Krebs_in_Deutschland_fuer_2013_2014.pdf. https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/kid_2017/krebs_in_deutschland_2017.pdf;jsessionid=4ABF74E94BB57BE2148A3647A84421BA.2_cid363?__blob=publicationFile. Accessed 3 Nov 2018
s2k_leitlinie_diagnostik-therapie-nachsorge-des-vaginalkarzinoms-und-seiner-vorstufen_2018–11.pdf. (2018) https://www.awmf.org/uploads/tx_szleitlinien/032-042l_S2k_Vaginalkarzinom-Vorstufen-Diagnostik-Therapie-Nachsorge_2018-11.pdf. Accessed 30 Oct 2018
Lamos C et al (2016) Detection of human papillomavirus infection in patients with vaginal intraepithelial neoplasia. PLoS ONE 11(12):e0167386
WHO Classification of Tumours of Female Reproductive Organs, 4th Edition, 2014.pdf. https://drzafariqbal.com/wp-content/uploads/2017/07/WHO-Female.pdf. Accessed 20 Apr 2018
Gunderson CC et al (2013) Vaginal cancer: the experience from 2 large academic centers during a 15-year period. J Low Genit Tract Dis 17(4):409–413
Smith JS et al (2009) Human papillomavirus type-distribution in vulvar and vaginal cancers and their associated precursors. Obstet Gynecol 113(4):917–924
Dovey de la Cour C et al (2019) Human papillomavirus types in cervical high-grade lesions or cancer among nordic women: potential for prevention. Cancer Med 8(2):839–849
Siegler E et al (2016) Vulvar and vaginal cancer, vulvar intraepithelial neoplasia 3 and vaginal intraepithelial neoplasia 3: experience of a referral institute. Isr Med Assoc J 18(5):286–289
Rhodes HE, Chenevert L, Munsell M (2014) Vaginal intraepithelial neoplasia (VaIN 2/3): comparing clinical outcomes of treatment with intravaginal estrogen. J Low Genit Tract Dis 18(2):115–121
Jakobsson M et al (2011) Cancer incidence among Finnish women with surgical treatment for cervical intraepithelial neoplasia, 1987–2006. Int J Cancer 128(5):1187–1191
Sopracordevole F et al (2015) Abnormal PAP-smear and diagnosis of high-grade vaginal intraepithelial neoplasia: a retrospective cohort study. Medicine (Baltimore) 94(42):e1827
Stuebs FA et al (2018) Accuracy of colposcopy-directed biopsy in detecting early cervical neoplasia: a retrospective study. Arch Gynecol Obstet 299(2):525–532
Baum ME et al (2006) Colposcopic accuracy of obstetrics and gynecology residents. Gynecol Oncol 103(3):966–970
Beckmann MW et al (2014) Establishment of the certification system "gynaecological dysplasia" in Germany. Geburtshilfe Frauenheilkd 74(9):860–867
Bornstein J et al (2012) 2011 colposcopic terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet Gynecol 120(1):166–172
Horn LC et al (2016) Nomenclature of squamous cell precursor lesions of the lower female genital tract : current aspects. Pathologe 37(6):526–533
Reich O et al (2015) Precancerous lesions of the cervix, vulva and vagina according to the 2014 WHO Classification of tumors of the female genital tract. Geburtshilfe Frauenheilkd 75(10):1018–1020
Graham K et al (2007) 20-year retrospective review of medium dose rate intracavitary brachytherapy in VAIN3. Gynecol Oncol 106(1):105–111
Chappatte OA et al (1991) Histological differences between colposcopic-directed biopsy and loop excision of the transformation zone (Letz): a Cause for Concern. Gynecol Oncol 43(1):46–50
Zhang X et al (2017) A retrospective analysis on 1901 women with high grade cervical intraepithelial neoplasia by colposcopic biopsy. Eur J Obstet Gynecol Reprod Biol 217:53–58
Burger MP, Hollema H (1993) The reliability of the histologic diagnosis in colposcopically directed biopsies. A plea for LETZ. Int J Gynecol Cancer 3(6):385–390
Barnes B et al (2016) RKI Bericht zum Krebsgeschehen in Deutschland 2016. https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebsgeschehen/Krebsgeschehen_node.html. Accessed 24 Oct 2018
De Vuyst H et al (2009) Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: a meta-analysis. Int J Cancer 124(7):1626–1636
Del Pino M, Rodriguez-Carunchio L, Ordi J (2013) Pathways of vulvar intraepithelial neoplasia and squamous cell carcinoma. Histopathology 62(1):161–175
Khan MJ et al (2016) A common clinical dilemma: management of abnormal vaginal cytology and human papillomavirus test results. Gynecol Oncol 141(2):364–370
Simoes E et al (2013) Cervical cancer screening: defining the need for research. Geburtshilfe Frauenheilkd 73(3):239–246
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (2007) Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum 90:1–636
Gunderson CC et al (2013) A contemporary analysis of epidemiology and management of vaginal intraepithelial neoplasia. Am J Obstet Gynecol 208(5):410.e1–6
Cong Q et al (2019) Importance of colposcopy impression in the early diagnosis of post hysterectomy vaginal cancer. J Low Genit Tract Dis 23(1):13–17
Rajaram S, Maheshwari A, Srivastava A (2015) Staging for vaginal cancer. Best Pract Res Clin Obstet Gynaecol 29(6):822–832
Author information
Authors and Affiliations
Contributions
FAS, MCK, MWB: Protocol/project development, Manuscript writing/editing. FAS, MCK, CES, GM, PG, AH and SKR: Data collection or management. FAS, MCK, MWB, WA, JS: Data analysis.
Corresponding author
Ethics declarations
Conflict of interest
P. Gass has received honoraria from Novartis, financial support for symposia from Novartis, Roche, and PharmaMar, and reimbursement of travel expenses from the discovering hands® company. None of the other authors have any conflicts of interest. Completed disclosure of conflict of interest forms are available for viewing online as supporting information.
Ethical approval
Approval for the study was obtained from the ethics committee of the Faculty of Medicine at Friedrich Alexander University of Erlangen-Nuremberg. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.Sources of funding support: no funding was received for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stuebs, F.A., Koch, M.C., Mehlhorn, G. et al. Accuracy of colposcopic findings in detecting vaginal intraepithelial neoplasia: a retrospective study. Arch Gynecol Obstet 301, 769–777 (2020). https://doi.org/10.1007/s00404-020-05441-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05441-5