Abstract
Objective
The vaginal microbiota may modulate susceptibility to Neisseria gonorrhea (NG) infections. The objective of this meta-analysis was to evaluate the association between these NG infections and the vaginal microbiota.
Method
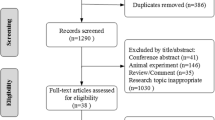
A systematic review and meta-analysis was conducted to investigate the correlation of vaginal microbiota and NG risk. Primary sources of the reviewed studies were from inception through December 2018. Vaginal mucosa microflora were dichotomized into high-Lactobacillus vaginal microbiota and low-Lactobacillus vaginal microbiota (LL-VMB), using either Nugent score, Amsel’s criteria, presence of clue cells or 16S rRNA gene sequencing.
Results
A total of 8 studies qualified for inclusion in this meta-analysis. LL-VMB could be regarded as worse prognostic factor, and the pooled OR was 1.33 (95% CI 1.02, 1.73; P = 0.04, I2 = 44%). LL-VMB was associated with a significantly higher susceptibility of NG. Trend for the sensitive analysis was consistence with the primary outcome. Significant publication bias was not detected by the funnel plot.
Conclusion
In conclusion, the systematic review and meta-analysis has demonstrated that LL-VMB was significantly associated with a high NG susceptibility.




Similar content being viewed by others
References
Kramer P, Bressan P (2015) Humans as superorganisms: how microbes, viruses, imprinted genes, and other selfish entities shape our behavior. Perspect Psychol Sci 10:464–481
van der Meulen TA, van Nimwegen JF, Harmsen HJM, Liefers SC, van der Tuuk K, Kroese FGM et al (2019) Normal vaginal microbiome in women with primary Sjögren's syndrome-associated vaginal dryness. Ann Rheum Dis 78:707–709
Greenbaum S, Greenbaum G, Moran-Gilad J, Weintruab AY (2019) Ecological dynamics of the vaginal microbiome in relation to health and disease. Am J Obstet Gynecol 220:324–335
Miller EA, Beasley DE, Dunn RR, Archie EA (2016) Lactobacilli dominance and vaginal pH: why is the human vaginal microbiome unique? Front Microbiol 7:1936
Freitas AC, Chaban B, Bocking A, Rocco M, Yang S, Hill JE, VOGUE Research Group et al (2017) The vaginal microbiome of pregnant women is less rich and diverse, with lower prevalence of Mollicutes, compared to non-pregnant women. Sci Rep 7:9212
Campisciano G, Florian F, D'Eustacchio A, Stanković D, Ricci G, De Seta F et al (2017) Subclinical alteration of the cervical-vaginal microbiome in women with idiopathic infertility. J Cell Physiol 232:1681–1688
Lewis FM, Bernstein KT, Aral SO (2017) Vaginal microbiome and its relationship to behavior, sexual health, and sexually transmitted diseases. Obstet Gynecol 129:643–654
Paramel Jayaprakash T, Wagner EC, van Schalkwyk J, Albert AY, Hill JE, Money DM, PPROM Study Group (2016) High diversity and variability in the vaginal microbiome in women following preterm premature rupture of membranes (PPROM): a prospective cohort study. PLoS ONE 11(11):e0166794
Gottschick C, Deng ZL, Vital M, Masur C, Abels C, Pieper DH et al (2017) Treatment of biofilms in bacterial vaginosis by an amphoteric tenside pessary-clinical study and microbiota analysis. Microbiome 5:119
Martin DH, Marrazzo JM (2016) The vaginal microbiome: current understanding and future directions. J Infect Dis 214(Suppl 1):S36–41
van de Wijgert JHHM (2017) The vaginal microbiome and sexually transmitted infections are interlinked: consequences for treatment and prevention. PLoS Med 14:e1002478
Schubert B, Maddamsetti R, Nyman J, Farhat MR, Marks DS (2018) Genome-wide discovery of epistatic loci affecting antibiotic resistance in Neisseria gonorrhoeae using evolutionary couplings. Nat Microbiol 4:328
Town K, Bolt H, Croxford S, Cole M, Harris S, Field N et al (2018) Neisseria gonorrhoeae molecular typing for understanding sexual networks and antimicrobial resistance transmission: a systematic review. J Infect 76:507–514
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. https://www.cochranehandbook.org. Accessed 24 Dec 2018
Comprehensive Meta Analysis (CMA) [Computer program] 2011 Version 2.0 Biostat Inc New Jersey.
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Abbai NS, Moodley P, Reddy T, Zondi TG, Rambaran S, Naidoo K et al (2015) Clinical evaluation of the OneStep Gonorrhea RapiCard InstaTest for detection of Neisseria gonorrhoeae in symptomatic patients from KwaZulu-Natal, South Africa. Microbiology 53:1348–1350
Francis SC, Ao TT, Vanobberghen FM, Chilongani J, Hashim R, Andreasen A, Watson-Jones D et al (2014) Epidemiology of curable sexually transmitted infections among women at increased risk for HIV in northwestern Tanzania: inadequacy of syndromic management. PLoS ONE 9:e101221
Brotman RM, Klebanoff MA, Nansel TR, Yu KF, Andrews WW, Zhang J et al (2010) Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J Infect Dis. 202:1907–1915
Kapiga S, Kelly C, Weiss S, Daley T, Peterson L, Leburg C et al (2009) Risk factors for incidence of sexually transmitted infections among women in South Africa, Tanzania, and Zambia: results from HPTN 055 study. Sex Transm Dis 36:199–206
Kaul R, Nagelkerke NJ, Kimani J, Ngugi E, Bwayo JJ, Macdonald KS, Kibera HIV Study Group et al (2007) Prevalent herpes simplex virus type 2 infection is associated with altered vaginal flora and an increased susceptibility to multiple sexually transmitted infections. J Infect Dis 196:1692–1697
Uma S, Balakrishnan P, Murugavel KG, Srikrishnan AK, Kumarasamy N, Cecelia JA et al (2005) Bacterial vaginosis in female sex workers in Chennai, India. Sex Health 2:261–262
Yen S, Shafer MA, Moncada J, Campbell CJ, Flinn SD, Boyer CB (2003) Bacterial vaginosis in sexually experienced and non-sexually experienced young women entering the military. Obstet Gynecol 102:927–933
Ness RB, Hillier SL, Richter HE, Soper DE, Stamm C, McGregor J et al (2002) Douching in relation to bacterial vaginosis, lactobacilli, and facultative bacteria in the vagina. Obstet Gynecol 100:765
Funding
This study was funded by Exploration on Comprehensive Prevention and Treatment of Syphilis in Guangzhou (20181A031003).
Author information
Authors and Affiliations
Contributions
JZ: Data collection, data analysis. RY: Data collection, data analysis. WH: Manuscript writing. XZ: Data collection, data analysis. WL: Manuscript writing. HZ: Data collection, data analysis. XZ: Manuscript writing. QL: Supervisor, Manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no competing interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zeng, J., Yang, R., He, W. et al. Modulation effect of vaginal mucosal microflora and susceptibility to Neisseria gonorrhoeae infections: a systematic review and meta-analysis. Arch Gynecol Obstet 300, 261–267 (2019). https://doi.org/10.1007/s00404-019-05200-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05200-1