Abstract
Purpose
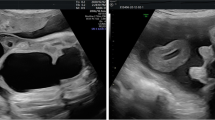
Isolated classic bladder exstrophy (CBE) is the most common variant of the bladder-exstrophy–epispadias complex (BEEC). The BEEC represents a spectrum ranging from isolated epispadias over CBE to the most severe form, cloacal exstrophy. We report on a series of 12 cases with CBE diagnosed prenatally and illustrate the spectrum of prenatal ultrasound findings with comparison to prior published reports on this entity.
Methods
This was a retrospective study involving 12 fetuses with CBE at two large tertiary referral centers in Germany over a 14-year period (2004–2018).
Results
Median diagnosis was made with ultrasound in 24 + 5 (IQR25,75: 21 + 2, 29 + 0) weeks of gestation. All fetuses presented with the pathognomonic findings non-visualization of the fetal bladder and protruding abdominal mass below the umbilical cord insertion. All fetuses showed normal kidney anatomy and normal amniotic fluid throughout pregnancy. Epispadia was visible prenatally on ultrasound in 6/8 male fetuses. 1/12 Parents opted for termination of pregnancy, 11/12 fetuses were live born and received reconstructive surgery.
Conclusions
Isolated CBE is an extremely rare prenatal sonographic finding. Prenatal diagnostics should exclude additional malformations within the spectrum of cloacal malformations.


Similar content being viewed by others
References
Ebert AK, Reutter H, Ludwig M, Rosch WH (2009) The exstrophy–epispadias complex. Orphanet J Rare Dis 4:23. https://doi.org/10.1186/1750-1172-4-23
Siffel C, Correa A, Amar E, Bakker MK, Bermejo-Sanchez E, Bianca S, Castilla EE, Clementi M, Cocchi G, Csaky-Szunyogh M, Feldkamp ML, Landau D, Leoncini E, Li Z, Lowry RB, Marengo LK, Mastroiacovo P, Morgan M, Mutchinick OM, Pierini A, Rissmann A, Ritvanen A, Scarano G, Szabova E, Olney RS (2011) Bladder exstrophy: an epidemiologic study from the International Clearinghouse for Birth Defects Surveillance and Research, and an overview of the literature. Am J Med Genet C Semin Med Genet 157C(4):321–332. https://doi.org/10.1002/ajmg.c.30316
Götz D, Hoffmann J, Köhn A, Rißmann A, Spillner C, Vogt C (2017) Fehlbildungsmonitoring Sachsen-Anhalt an der Medizinischen Fakultät der Otto-von-Guericke-Universität Magdeburg. https://www.angeborene-fehlbildungen.com/monz_mm/Dokumente/Jahresberichte/Bericht2017_WEB.pdf. Accessed 25 Apr 2019
Carey JC (2001) Exstrophy of the cloaca and the OEIS complex: one and the same. Am J Med Genet 99(4):270
Mallmann MR, Reutter H, Geipel A, Berg C, Gembruch U (2014) Early prenatal diagnosis of the OEIS complex with different appearance in early compared with late pregnancy before spontaneous rupture of the cloacal membrane. Prenat Diagn 34(8):803–805. https://doi.org/10.1002/pd.4355
Mallmann MR, Reutter H, Muller A, Boemers TM, Geipel A, Berg C, Gembruch U (2014) Prenatal diagnosis of covered cloacal exstrophy. Fetal Diagn Ther 36(4):333–336. https://doi.org/10.1159/000360418
Mallmann MR, Reutter H, Muller AM, Geipel A, Berg C, Gembruch U (2017) Omphalocele–exstrophy–imperforate anus-spinal defects complex: associated malformations in 12 new cases. Fetal Diagn Ther 41(1):66–70. https://doi.org/10.1159/000446108
Cacciari A, Pilu GL, Mordenti M, Ceccarelli PL, Ruggeri G (1999) Prenatal diagnosis of bladder exstrophy: what counseling? J Urol 161(1):259–261
Lee EH, Shim JY (2003) New sonographic finding for the prenatal diagnosis of bladder exstrophy: a case report. Ultrasound Obstet Gynecol 21(5):498–500. https://doi.org/10.1002/uog.114
Jaffe R, Schoenfeld A, Ovadia J (1990) Sonographic findings in the prenatal diagnosis of bladder exstrophy. Am J Obstet Gynecol 162(3):675–678
Gearhart JP, Ben-Chaim J, Jeffs RD, Sanders RC (1995) Criteria for the prenatal diagnosis of classic bladder exstrophy. Obstet Gynecol 85(6):961–964. https://doi.org/10.1016/0029-7844(95)00069-4
Pinette MG, Pan YQ, Pinette SG, Stubblefield PG, Blackstone J (1996) Prenatal diagnosis of fetal bladder and cloacal exstrophy by ultrasound A report of three cases. J Reprod Med 41(2):132–134
Wolniakowski A, Szlachetka K (2014) Prenatal diagnosis of bladder exstrophy. J Diagnos Med Sonogr 30(2):88–91
Goldstein I, Shalev E, Nisman D (2001) The dilemma of prenatal diagnosis of bladder exstrophy: a case report and a review of the literature. Ultrasound Obstet Gynecol 17(4):357–359. https://doi.org/10.1046/j.1469-0705.2001.00274.x
Tong SY, Lee JE, Kim SR, Lee SK (2007) Umbilical cord cyst: a prenatal clue to bladder exstrophy. Prenat Diagn 27(12):1177–1179. https://doi.org/10.1002/pd.1872
Antomarchi J, Moeglin D, Laurichesse H, Combourieu D, Bigi N, Maisonneuve E, Legac P, Althuser M, Delotte J, Jouannic JM, Bongain A (2018) The pubic diastasis measurement, a key element for the diagnosis, management, and prognosis of the bladder exstrophy. Fetal Diagn Ther. https://doi.org/10.1159/000492817
Fishel-Bartal M, Perlman S, Messing B, Bardin R, Kivilevitch Z, Achiron R, Gilboa Y (2017) Early diagnosis of bladder exstrophy: quantitative assessment of a low-inserted umbilical cord. J Ultrasound Med 36(9):1801–1805. https://doi.org/10.1002/jum.14212
Bronshtein M, Gilboa Y, Gover A, Beloosesky R (2017) Direct lower abdominal ureteral jet as sonographic sign of bladder exstrophy. Ultrasound Obstet Gynecol 49(3):412–413. https://doi.org/10.1002/uog.15906
Evangelidis A, Murphy JP, Gatti JM (2004) Prenatal diagnosis of bladder exstrophy by 3-dimensional ultrasound. J Urol 172(3):1111. https://doi.org/10.1097/01.ju.0000135595.83972.6a
Hsieh K, O'Loughlin MT, Ferrer FA (2005) Bladder exstrophy and phenotypic gender determination on fetal magnetic resonance imaging. Urology 65(5):998–999. https://doi.org/10.1016/j.urology.2004.12.060
Goldman S, Szejnfeld PO, Rondon A, Francisco VV, Bacelar H, Leslie B, Barroso U Jr, Ortiz V, Macedo A Jr (2013) Prenatal diagnosis of bladder exstrophy by fetal MRI. J Pediatr Urol 9(1):3–6. https://doi.org/10.1016/j.jpurol.2012.06.018
Draaken M, Baudisch F, Timmermann B, Kuhl H, Kerick M, Proske J, Wittler L, Pennimpede T, Ebert AK, Rosch W, Stein R, Bartels E, von Lowtzow C, Boemers TM, Herms S, Gearhart JP, Lakshmanan Y, Kockum CC, Holmdahl G, Lackgren G, Nordenskjold A, Boyadjiev SA, Herrmann BG, Nothen MM, Ludwig M, Reutter H (2014) Classic bladder exstrophy: frequent 22q11.21 duplications and definition of a 414 kb phenocritical region. Birth Defects Res A Clin Mol Teratol 100(6):512–517. https://doi.org/10.1002/bdra.23249
Jochault-Ritz S, Mercier M, Aubert D (2010) Short and long-term quality of life after reconstruction of bladder exstrophy in infancy: preliminary results of the QUALEX (QUAlity of Life of bladder EXstrophy) study. J Pediatr Surg 45(8):1693–1700. https://doi.org/10.1016/j.jpedsurg.2010.03.032
Shaw MB, Rink RC, Kaefer M, Cain MP, Casale AJ (2004) Continence and classic bladder exstrophy treated with staged repair. J Urol 172(4 Pt 1):1450–1453 (Discussion 1453)
Ansari MS, Cervellione RM, Gearhart JP (2010) Sexual function and fertility issues in cases of exstrophy epispadias complex. Indian J Urol 26(4):595–597. https://doi.org/10.4103/0970-1591.74477
Mirk P, Calisti A, Fileni A (1986) Prenatal sonographic diagnosis of bladder extrophy. J Ultrasound Med 5(5):291–293
Barth RA, Filly RA, Sondheimer FK (1990) Prenatal sonographic findings in bladder exstrophy. J Ultrasound Med 9(6):359–361
Erb R, Jaffe R, Braren V, Jeanty P (1992) Exstrophy of the cloaca sequence. The fetus.net. https://sonoworld.com/TheFetus/page.aspx?id=569. Accessed 5 Dec 2018
Bronshtein M, Bar-Hava I, Blumenfeld Z (1993) Differential diagnosis of the nonvisualized fetal urinary bladder by transvaginal sonography in the early second trimester. Obstet Gynecol 82(4 Pt 1):490–493
Messelink EJ, Aronson DC, Knuist M, Heij HA, Vos A (1994) Four cases of bladder exstrophy in two families. J Med Genet 31(6):490–492
Khandelwal M, Coyman RC, Barahona O, Schmitt R, Reece EA (1996) Early prenatal diagnosis of bladder exstrophy: case report and review of the literature. Fetal Diagn Ther 11(2):146–149. https://doi.org/10.1159/000264294
Mabille M, De Laveaucoupet J, Senat MV, Picone O, Levaillant JM, Mas AE, Musset D (2009) Imaging of the fetal bony pelvis by computed tomography in a case of bladder exstrophy. Ultrasound Obstet Gynecol 33(6):716–719. https://doi.org/10.1002/uog.6409
Author information
Authors and Affiliations
Contributions
MRM: project development, data collection, data analysis, manuscript writing. BM-D: data collection, data analysis. HR: data analysis, data analysis, manuscript writing. RP: data collection, manuscript editing. IG: data collection, data analysis, manuscript editing. AG: data collection, data analysis, manuscript editing. CB: data collection, data analysis, manuscript editing. TMB: project development, data collection, manuscript writing. UG: project development, data collection, data analysis, manuscript writing. All authors finally approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mallmann, M.R., Mack-Detlefsen, B., Reutter, H. et al. Isolated bladder exstrophy in prenatal diagnosis. Arch Gynecol Obstet 300, 355–363 (2019). https://doi.org/10.1007/s00404-019-05193-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05193-x