Abstract
Purpose
(1) To evaluate the association between immigration background and the occurrence of maternal near miss (MNM). (2) To identify medical co-factors, health-care utilization, and health-care disparities as explanations of a possibly higher risk of MNM among immigrants.
Methods
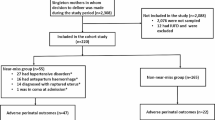
We compared perinatal outcomes between immigrant women (first- or second-generation) versus non-immigrant women, delivering at three maternity hospitals in Berlin, Germany, 2011–2012. Near-miss events were defined as: HELLP syndrome, eclampsia, the occurrence or threat of uterine rupture, postpartum hemorrhage (PPH) > 1000 ml, sepsis, peripartal hysterectomy, cardiovascular complications, lung embolism. Logistic regression analyses were performed to determine the associations of immigration status, acculturation, and language competency with near-miss events, and of near-miss events with the perinatal outcomes.
Results
The databank included 2647 first-generation immigrants, 889 second-generation immigrants, and 3231 women without an immigration background (total N = 6767). Near-miss events occurred in 141 women. The likelihood of near-miss events was lower among multiparous women (OR 0.6; 95% CI 0.42–0.87; p = 0.01). No other factors had a statistically significant influence. Near-miss events are associated with an elevated likelihood for an unfavorable perinatal condition: the ORs ranged from 2.15 for an arterial umbilical cord pH value < 7.1–2.47 for premature delivery.
Conclusions
Immigration status does not change the risk of near-miss events. Besides parity, no medical or socio-demographic factors were identified that were associated with an elevated likelihood for the occurrence of severe peripartal complications.
Similar content being viewed by others
References
Adeoye IA, Onayade AA, Fatusi AO (2013) Incidence, determinants and perinatal outcomes of near miss maternal morbidity in Ile-Ife Nigeria: a prospective case control study. BMC Pregnancy Childbirth 13(1):93
Bongard S, Arslaner H, Pogge SF (2000) Acculturation and cardiovascular reactivity of secondgeneration—Turkish migrants in Germany. J Psychosom Res 53:795–803 (FRAKK-Fragebogeninstrument, o. O Bongard S, Pogge SF, Arslaner H, Rohrmann S, Hodapp V (2002))
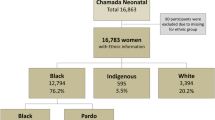
Fernandes KG, Souza RT, Carmo Leal M, Moura EC, Santos LM, Cecatti JG (2017) Ethnic differences in maternal near miss. Arch Gynecol Obstet 296:1063–1070
Geller SE, Koch AR, Garland CE, MacDonald EJ, Storey F, Lawton B (2018) A global view of severe maternal morbidity: moving beyond maternal mortality. Reprod Health 15(Suppl 1):98. https://doi.org/10.1186/s12978-018-0527-2
Jonkers M, Richters A, Zwart J, Öry F, van Roosmalen J (2011) Severe maternal morbidity among immigrant women in the Netherlands: patients’ perspectives. Reprod Health Matters 19:144–153
Knight M, Kurinczuk JJ, Spark P, Brocklehurst P (2009) Inequalities in maternal health: national cohort study of ethnic variation in severe maternal morbidities. BMJ 338:b542
Liyew EF, Yalew AW, Afework MF, Essen B (2018) Maternal near-miss and the risk of adverse perinatal outcomes: a prospective cohort study in selected public hospitals of Addis Ababa Ethiopia. BMC Pregnancy Childbirth 18:345. https://doi.org/10.1186/s12884-018-1983-y
Nair M, Kurinczuk JJ, Knight M (2014) Ethnic variations in severe maternal morbidity in the UK—a case-control study. PLoS One 9(4):e95086
Nardello DM, Guimarães AMDAN, Barreto IDC, Gurgel RQ, Ribeiro ERO, Gois CFL (2017) Fetal and neonatal deaths of children of patients classified as near miss. Rev Bras Enferm 70(1):98–105
Neuhaus ST, Bremerich D (2018) Schwangerschaft- und Geburtsrisiken. In: Kranke P (ed.) Die geburtshilfliche Anästhesie. Springer, Berlin, p 42–62. http://www.springer.com/978-3-662-54374-0. Accessed 15 Oct 2018
Oliveira LC, Costa AAR (2013) Óbitos fetais e neonatais entre casos de near miss materno [fetal and neonatal deaths among cases of maternal near miss]. Rev Assoc Med Bras 59(5):487–494
Reime B, Janssen PA, Farris L, Borde T, Hellmers C et al (2012) Maternal near-miss among women with a migrant background in Germany. Acta Obstet Gynecol Scand 91:824–829
Say L, Pattinson RC, Gülmezoglu AM (2004) WHO systematic review of maternal morbidity and mortality: the prevalence of severe acute maternal morbidity (near miss). Reprod Health 1:3. https://doi.org/10.1186/1742-4755-1-3
Say L, Souza JP, Pattinson RC (2009) Maternal near miss towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol 23(3):287–296
Schenk L, Bau AM, Borde T, Butler J, Lampert T, Neuhauser H, Razum O, Weilandt C (2006) Mindestindikatorensatz zur Erfassung des Migrationsstatus. Empfehlungen für die epidemiologische Praxis. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 49:853–860
Souza JP, Cecatti JG, Faundes A, Morais SS, Villar J, Carroli G, Gulmezoglu M, Wojdyla D, Zavaleta N, Donner A et al (2010) Maternal near miss and maternal death in the World Health Organization's 2005 global survey on maternal and perinatal health. Bull World Health Organ 88(2):113–119
The World Health Organization [WHO] (2011) Evaluating the quality of care for severe pregnancy complications. In: The WHO near-miss approach for maternal health. Geneva, Switzerland
Waterstone M, Bewley S, Wolfe C (2001) Incidence and predictors of severe obstetric morbidity: case-control study. BMJ 322:1089–1094
Zanardi DM, Parpinelli MA, Haddad SM, Costa ML, Sousa MH, Leite FBD, Cecatti JG (2018) Adverse perinatal outcomes are associated with severe maternal morbidity and mortality: evidence from a national multicentre cross-sectional study. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-018-5004-1
Zwart JJ, Jonkers MD, Richters A, Öry F, Bloemenkamp KW et al (2011) Ethnic disparity in severe acute maternal morbidity: a nationwide cohort study in the Netherlands. Eur J Public Health 21:229–234
Acknowledgements
We would like to thank Michael Hanna, PhD (Mercury Medical Research and Writing), for translating the manuscript from German to English.
Funding
This study was supported by Deutsche Forschungsgemeinschaft (Grant No. FKZ: DA 1199/2-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
David, M., Razum, O., Henrich, W. et al. The impact of migration background on maternal near miss. Arch Gynecol Obstet 300, 285–292 (2019). https://doi.org/10.1007/s00404-019-05179-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05179-9