Abstract
Purpose
To characterize and understand the demographics (age and body mass index, BMI) of a cohort of women who delivered at a single institution over an 11-year period. The purpose of this analysis is to look for effects over time of demographic characteristics on mode of delivery.
Methods
Retrospective analysis of singleton deliveries between 2004–2014, n = 27,729; level 1 perinatal center, university hospital setting. Data were extracted from the digital birth registry. All statistical analyses were done using R version 3.5.1. Variables analyzed were: age, BMI, and mode of delivery (in the current and any prior pregnancies).
Results
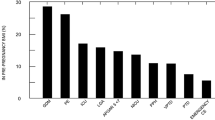
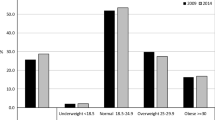
Mean age increased from 31.1 ± 5.2 years in 2004 to 31.5 ± 5.0 years in 2014 (p < 0.001, eta2 = 0.0006). Mean BMI before pregnancy increased from 23.7 ± 4.5 to 24.7 ± 5.2 kg/m2. Mean BMI at delivery increased from 28.5 ± 4.7 to 29.6 ± 5.2 kg/m2 (p < 0.001, eta2 = 0.0049). Regarding maternal age, patients with elective Cesarean section (CS) (32.5 ± 5.3 years), emergency CS (31.6 ± 5.6 years) and CS in labor (31.4 ± 5.3 years) were older compared to those with spontaneous (31.0 ± 5.2 years) or instrument-assisted vaginal delivery such as vacuum (31.0 ± 5.0 years) and forceps (30.2 ± 5.4 years). Among the multiparous patients, the mode of delivery in prior pregnancies is the variable with the greatest effect on the mode of delivery in any subsequent pregnancies. The mode of delivery was: spontaneous (55.5%), vaginal operative including vacuum and forceps (8.8%), and Cesarean section (35.7%).
Conclusions
Increase of age and BMI over years is significant, but very small and in a range which seems not clinically relevant. Previous births have the strongest effects on mode of delivery in the current pregnancy.

Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CS:
-
Cesarean section
- PFD:
-
Pelvic floor disorders
- WHO:
-
World Health Organization
References
Statistisches Bundesamt. Krankenhausentbindungen in Deutschland—Jahre 1991–2015. https://www.destatis.de/DE/ZahlenFakten/GesellschaftStaat/Gesundheit/Krankenhaeuser/Tabellen/KrankenhausentbindeungenKaiserschnitt.htm. Accessed June 2018
Huebner M, Brucker SY, Tunn R, Naumann G, Reisenauer C, Abele H (2017) Intrapartal pelvic floor protection: a pragmatic and interdisciplinary approach between obstetrics and urogynecology. Arch Gynecol Obstet 295(4):795–798. https://doi.org/10.1007/s00404-017-4316-x
Bihler J, Tunn R, Reisenauer C, Pauluschke-Frohlich J, Wagner P, Abele H, Rall KK, Naumann G, Wallwiener M, Brucker SY, Hubner M (2017) Personal preference of mode of delivery. What do urogynaecologists choose? Preliminary results of the DECISION Study. Geburtshilfe Frauenheilkd 77(11):1182–1188. https://doi.org/10.1055/s-0043-120919
Betran AP, Torloni MR, Zhang JJ, Gulmezoglu AM, Section WHOWGoC (2016) WHO Statement on Caesarean Section Rates. BJOG 123(5):667–670. https://doi.org/10.1111/1471-0528.13526
World Health Organization Human Reproduction Programme A (2015) WHO statement on caesarean section rates. Reprod Health Matters 23(45):149–150. https://doi.org/10.1016/j.rhm.2015.07.007
Wehberg S, Guldberg R, Gradel KO, Kesmodel US, Munk L, Andersson CB, Jolving LR, Nielsen J, Norgard BM (2018) Risk factors and between-hospital variation of caesarean section in Denmark: a cohort study. BMJ Open 8(2):e019120. https://doi.org/10.1136/bmjopen-2017-019120
Fahmy WM, Crispim CA, Cliffe S (2018) Association between maternal death and cesarean section in Latin America: a systematic literature review. Midwifery 59:88–93. https://doi.org/10.1016/j.midw.2018.01.009
Bermudez-Tamayo C, Johri M, Chaillet N (2018) Budget impact of a program for safely reducing caesarean sections in Canada. Midwifery 60:20–26. https://doi.org/10.1016/j.midw.2018.01.022
Lucas DN, Yentis SM, Kinsella SM, Holdcroft A, May AE, Wee M, Robinson PN (2000) Urgency of caesarean section: a new classification. J R Soc Med 93(7):346–350. https://doi.org/10.1177/014107680009300703
Poobalan AS, Aucott LS, Gurung T, Smith WC, Bhattacharya S (2009) Obesity as an independent risk factor for elective and emergency caesarean delivery in nulliparous women—systematic review and meta-analysis of cohort studies. Obes Rev 10(1):28–35. https://doi.org/10.1111/j.1467-789X.2008.00537.x
Breart G (1997) Delayed childbearing. Eur J Obstet Gynecol Reprod Biol 75(1):71–73
Sandall J (2015) Place of birth in Europe. Entre Nous The Eur Mag Sexual Reprod Health 81:16–17
Norman JE, Stock SJ (2018) Birth options after a caesarean section. BMJ 360:j5737. https://doi.org/10.1136/bmj.j5737
Castiglioni L, Schmiedeberg C (2018) Joint effect of education and age at childbirth on the risk of caesarean delivery: findings from Germany 2008–2015. Public Health 155:1–7. https://doi.org/10.1016/j.puhe.2017.10.020
Begum T, Rahman A, Nababan H, Hoque DME, Khan AF, Ali T, Anwar I (2017) Indications and determinants of caesarean section delivery: evidence from a population-based study in Matlab, Bangladesh. PLoS ONE 12(11):e0188074. https://doi.org/10.1371/journal.pone.0188074
Caudwell-Hall J, Kamisan Atan I, Brown C, Guzman Rojas R, Langer S, Shek KL, Dietz HP (2018) Can pelvic floor trauma be predicted antenatally? Acta Obstet Gynecol Scand. https://doi.org/10.1111/aogs.13315
Glazener C, Elders A, Macarthur C, Lancashire RJ, Herbison P, Hagen S, Dean N, Bain C, Toozs-Hobson P, Richardson K, McDonald A, McPherson G, Wilson D, ProLong Study G (2013) Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG 120(2):161–168. https://doi.org/10.1111/1471-0528.12075
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ, Pelvic Floor Disorders N (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300(11):1311–1316. https://doi.org/10.1001/jama.300.11.1311
Jelovsek JE, Chagin K, Gyhagen M, Hagen S, Wilson D, Kattan MW, Elders A, Barber MD, Areskoug B, MacArthur C, Milsom I (2018) Predicting risk of pelvic floor disorders 12 and 20 years after delivery. Am J Obstet Gynecol 218(2):222. https://doi.org/10.1016/j.ajog.2017.10.014 (e221–222 e219)
Wilson D, Dornan J, Milsom I, Freeman R (2014) UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J 25(11):1449–1452. https://doi.org/10.1007/s00192-014-2376-z
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120(2):152–160. https://doi.org/10.1111/1471-0528.12020
Acknowledgements
The authors acknowledge all participating staff who entered data into the birth registry.
Funding
There was no funding.
Author information
Authors and Affiliations
Contributions
MH: project development, ethical approval, data acquisition, statistical analysis, manuscript writing/editing, project supervision. HA: project development, data acquisition, manuscript writing/editing, project supervision. CR: manuscript writing/editing. KK: project development, manuscript writing/editing. MHO: project development, manuscript writing/editing. PW: manuscript writing/editing. JPF: manuscript writing/editing. BS: statistical analysis, manuscript writing/editing. SYB: project supervision, manuscript writing/editing. KR: project development, statistical analysis, manuscript writing/editing, project supervision.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Ethical approval
The study was approved by the local ethics committee (Ethics Committee, Department of Medicine, Eberhard Karls University and University Hospital Tuebingen, Germany; 750/2017BO2, 27.11.2017). According to the committee´s guidelines, there is no informed consent of participants required, since this is a retrospective analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
About this article
Cite this article
Huebner, M., Abele, H., Reisenauer, C. et al. Demographic changes and effects on the mode of delivery: a retrospective analysis of a large birth registry containing 27,729 singleton deliveries in a level I center. Arch Gynecol Obstet 299, 747–754 (2019). https://doi.org/10.1007/s00404-019-05073-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05073-4