Abstract
Purpose
To analyze fetal cerebral malformations with late termination of pregnancy (TOP) and to evaluate the rate of cases that could have been detected earlier using international recommended requirements of sonographic examination of the fetal central nervous system (CNS).
Materials and methods
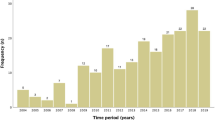
Cases of singleton pregnancies above 18 + 0 weeks of gestation ending in late TOP due to fetal CNS malformations between 2002 and 2011 were retrospectively reviewed. The cases were divided into isolated and non-isolated cerebral malformations. Prevalence and timing of TOP were assessed relative to the identified malformations.
Results
During this 10-year period, 212 (20.8%) out of 1017 late TOPs were performed in pregnancies with fetal cerebral malformations. 59 cases were excluded because of chromosomal anomalies. 86 (56.2%) of the remaining 153 cases were isolated cerebral malformations while 67 (43.8%) were non-isolated. TOP after viability (≥ 24 + 0 weeks of gestation) was performed in 61.4% (94/153). Substantial morbidity (n = 80; 52.3%) and mental retardation (n = 33, 38.4%) made up the leading prognostic groups. In about 80% of detectable anomalies, diagnosis of CNS malformation could have been made earlier by following international guidelines of fetal CNS examination at second trimester scan.
Conclusion
General implementation of ultrasound screening in maternity care can significantly reduce the number of late TOPs in Germany.
Similar content being viewed by others
References
Dommergues M, Mandelbrot L, Mahieu-Caputo D, Boudjema N, Durand-Zaleski I, foetale ICIG-Cdm (2010) Termination of pregnancy following prenatal diagnosis in France: how severe are the foetal anomalies? Prenat Diagn 30(6):531–539. https://doi.org/10.1002/pd.2510
Vaknin Z, Lahat Y, Barel O, Ben-Ami I, Reish O, Herman A, Maymon R (2009) Termination of pregnancy due to fetal abnormalities performed after 23 weeks’ gestation: analysis of indications in 144 cases from a single medical center. Fetal Diagn Ther 25(2):291–296. https://doi.org/10.1159/000229501
Barel O, Vaknin Z, Smorgick N, Reish O, Mendlovic S, Herman A, Maymon R (2009) Fetal abnormalities leading to third trimester abortion: nine-year experience from a single medical center. Prenat Diagn 29(3):223–228. https://doi.org/10.1002/pd.2188
Monteagudo A, Timor-Tritsch IE (2009) Normal sonographic development of the central nervous system from the second trimester onwards using 2D, 3D and transvaginal sonography. Prenat Diagn 29(4):326–339. https://doi.org/10.1002/pd.2146
Rouleau C, Gasner A, Bigi N, Couture A, Perez MJ, Blanchet P, Faure JM, Rivier F, Boulot P, Laquerriere A, Encha-Razavi F (2011) Prevalence and timing of pregnancy termination for brain malformations. Arch Dis Child Fetal Neonatal Ed 96(5):F360–F364. https://doi.org/10.1136/adc.2010.201483
Salomon LJ, Alfirevic Z, Berghella V, Bilardo C, Hernandez-Andrade E, Johnsen SL, Kalache K, Leung KY, Malinger G, Munoz H, Prefumo F, Toi A, Lee W, Committee ICS (2011) Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 37(1):116–126. https://doi.org/10.1002/uog.8831
International Society of Ultrasound in O, Gynecology Education C (2007) Sonographic examination of the fetal central nervous system: guidelines for performing the ‘basic examination’ and the ‘fetal neurosonogram’. Ultrasound Obstet Gynecol 29(1):109–116. https://doi.org/10.1002/uog.3909
Yinon Y, Katorza E, Nassie DI, Ben-Meir E, Gindes L, Hoffmann C, Lipitz S, Achiron R, Weisz B (2013) Late diagnosis of fetal central nervous system anomalies following a normal second trimester anatomy scan. Prenat Diagn 33(10):929–934. https://doi.org/10.1002/pd.4163
Korenromp MJ, Page-Christiaens GC, van den Bout J, Mulder EJ, Hunfeld JA, Potters CM, Erwich JJ, van Binsbergen CJ, Brons JT, Beekhuis JR, Omtzigt AW, Visser GH (2007) A prospective study on parental coping 4 months after termination of pregnancy for fetal anomalies. Prenat Diagn 27(8):709–716. https://doi.org/10.1002/pd.1763
den Hollander NS, Vinkesteijn A, Schmitz-van Splunder P, Catsman-Berrevoets CE, Wladimiroff JW (1998) Prenatally diagnosed fetal ventriculomegaly; prognosis and outcome. Prenat Diagn 18(6):557–566
Domröse CM, Bremer S, Buczek C, Geipel A, Berg C, Gembruch U, Willruth A (2016) Termination of pregnancy after prenatal diagnosis of spina bifida: a German perspective. Arch Gynecol Obstet 294(4):731–737. https://doi.org/10.1007/s00404-016-4032-y
Corbacioglu A, Aslan H, Aydin S, Akbayir O, Ersan F, Alpay V, Dagdeviren H, Kisacik S (2012) Trends in fetal indications for termination of pregnancy between 2002 and 2010 at a tertiary referral centre. J Turk Ger Gynecol Assoc 13(2):85–90. https://doi.org/10.5152/jtgga.2012.09
Pasquini L, Pontello V, Kumar S (2007) P47.08 Late termination of pregnancy: six years experience in a single United Kingdom tertiary centre. Ultrasound Obstet Gynecol 30:635
Carroll SG, Porter H, Abdel-Fattah S, Kyle PM, Soothill PW (2000) Correlation of prenatal ultrasound diagnosis and pathologic findings in fetal brain abnormalities. Ultrasound Obstet Gynecol 16(2):149–153. https://doi.org/10.1046/j.1469-0705.2000.00199.x
Garne E, Loane M, Dolk H, De Vigan C, Scarano G, Tucker D, Stoll C, Gener B, Pierini A, Nelen V, Rosch C, Gillerot Y, Feijoo M, Tincheva R, Queisser-Luft A, Addor MC, Mosquera C, Gatt M, Barisic I (2005) Prenatal diagnosis of severe structural congenital malformations in Europe. Ultrasound Obstet Gynecol 25(1):6–11. https://doi.org/10.1002/uog.1784
Dommergues M, Benachi A, Benifla JL, des Noettes R, Dumez Y (1999) The reasons for termination of pregnancy in the third trimester. Br J Obstet Gynaecol 106(4):297–303
Ouahba J, Luton D, Vuillard E, Garel C, Gressens P, Blanc N, Elmaleh M, Evrard P, Oury JF (2006) Prenatal isolated mild ventriculomegaly: outcome in 167 cases. BJOG 113(9):1072–1079. https://doi.org/10.1111/j.1471-0528.2006.01050.x
Rossi AC, Prefumo F (2013) Accuracy of ultrasonography at 11–14 weeks of gestation for detection of fetal structural anomalies: a systematic review. Obstet Gynecol 122(6):1160–1167. https://doi.org/10.1097/AOG.0000000000000015
Pilu G, Segata M, Ghi T, Carletti A, Perolo A, Santini D, Bonasoni P, Tani G, Rizzo N (2006) Diagnosis of midline anomalies of the fetal brain with the three-dimensional median view. Ultrasound Obstet Gynecol 27(5):522–529. https://doi.org/10.1002/uog.2751
Ghi T, Carletti A, Contro E, Cera E, Falco P, Tagliavini G, Michelacci L, Tani G, Youssef A, Bonasoni P, Rizzo N, Pelusi G, Pilu G (2010) Prenatal diagnosis and outcome of partial agenesis and hypoplasia of the corpus callosum. Ultrasound Obstet Gynecol 35(1):35–41. https://doi.org/10.1002/uog.7489
Grandjean H, Larroque D, Levi S (1999) The performance of routine ultrasonographic screening of pregnancies in the Eurofetus study. Am J Obstet Gynecol 181(2):446–454
Rüland AM, Berg C, Gembruch U, Geipel A (2015) Prenatal diagnosis of anomalies of the corpus callosum over a 13-year period. Ultraschall Med. https://doi.org/10.1055/s-0035-1553665
Ecker JL, Shipp TD, Bromley B, Benacerraf B (2000) The sonographic diagnosis of Dandy-Walker and Dandy-Walker variant: associated findings and outcomes. Prenat Diagn 20(4):328–332
Kolble N, Wisser J, Kurmanavicius J, Bolthauser E, Stallmach T, Huch A, Huch R (2000) Dandy-walker malformation: prenatal diagnosis and outcome. Prenat Diagn 20(4):318–327
Adama van Scheltema PN, Nagel HT, Brouwer OF, Vandenbussche FP (2003) Outcome of children with prenatally diagnosed central nervous system malformations. Ultrasound Obstet Gynecol 21(1):41–47. https://doi.org/10.1002/uog.6
Kuppermann M, Feeny D, Gates E, Posner SF, Blumberg B, Washington AE (1999) Preferences of women facing a prenatal diagnostic choice: long-term outcomes matter most. Prenat Diagn 19(8):711–716
Timor-Tritsch IE, Monteagudo A, Pilu G, Malinger G (2012) Ultrasonography of the prenatal and neonatal brain, 3rd, ed edn. McGraw-Hill Medical Publishing Division, New York
Richtlinien des Gemeinsamen Bundesausschusses über die ärztliche Betreuung während der Schwangerschaft und nach der Entbindung („Mutterschafts-Richtlinien“). veröffentlicht im Bundesanzeiger Nr. 126 vom 11. Juli 2003
Richtlinien des Gemeinsamen Bundesausschusses über die ärztliche Betreuung während der Schwangerschaft und nach der Entbindung („Mutterschafts-Richtlinien“) (2013). veröffentlicht im Bundesanzeiger AT 29.05.2013 B5
Merz E, Eichhorn KH, von Kaisenberg C, Schramm T, der Arbeitsgruppe D-S III (2012) Updated quality requirements regarding secondary differentiated ultrasound examination in prenatal diagnostics (= DEGUM level II) in the period from 18 + 0 to 21 + 6 weeks of gestation. Ultraschall Med 33(6):593–596. https://doi.org/10.1055/s-0032-1325500
Cargill Y, Morin L, Diagnostic Imaging C (2009) Content of a complete routine second trimester obstetrical ultrasound examination and report. J Obstet Gynaecol Can 31(3):272–275. https://doi.org/10.1016/S1701-2163(16)34127-5
National Collaborating Centre for Women's and Children's Health (UK) (2008) Antenatal care: routine care for the healthy pregnant woman. National Institute for Health and Clinical Excellence: Guidance. RCOG Press, London
Committee on Practice B-O, The American Institute of Ultrasound in M (2016) Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol 128(6):e241–e256. https://doi.org/10.1097/aog.0000000000001815
Funding
None.
Author information
Authors and Affiliations
Contributions
CD Manuscript writing, project development, data analysis, SB data collection and management, CB data collection and management, AG investigation, CB Investigation, AH investigation, UG project development, manuscript editing, AW manuscript editing, project development, data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This is a retrospective study of data routinely achieved and anonymously analyzed. Our local ethics committee (Ethikkommission an der Medizinischen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn) does not generate a protocol in this form of study but frees us from it. All findings were extracted from the medical records and stored in an anonymized data base.
Rights and permissions
About this article
Cite this article
Domröse, C.M., Bremer, S., Buczek, C. et al. Termination of pregnancy following prenatally diagnosed central nervous system malformations. Arch Gynecol Obstet 298, 903–910 (2018). https://doi.org/10.1007/s00404-018-4900-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4900-8