Abstract
Objective
To investigate the association between episiotomy and perineal damage in the subsequent delivery.
Study design
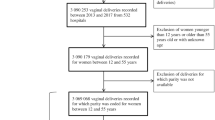
A retrospective cohort study was conducted, comparing outcome of subsequent singleton deliveries of women with and without episiotomy in their first (index) delivery. Deliveries occurred between the years 1991–2015 in a tertiary medical center. Traumatic vaginal tears, multiple pregnancies, and cesarean deliveries (CD) in the index pregnancy were excluded from the analysis. Multiple logistic regression models were used to control for confounders.
Results
During the study period, 43,066 women met the inclusion criteria; of them, 50.4% (n = 21,711) had subsequent delivery after episiotomy and 49.6% (n = 21,355) had subsequent delivery without episiotomy in the index pregnancy. Patients with episiotomy in the index birth higher rates of subsequent episiotomy (17.5 vs. 3.1%; P < 0.001; OR 1.9; 95% CI). In addition, the rates of the first and second degree perineal tears as well as the third and fourth degree perineal tears were significantly higher in patients following episiotomy (33.6 vs. 17.8%; P < 0.001, and 0.2 vs. 0.1%; P = 0.002, respectively). Nevertheless, there was no significant difference at the rates of CD and instrumental deliveries, between the groups. While adjusting for maternal age, ethnicity, birth weight, and vacuum delivery—the previous episiotomy was noted as an independent risk factor for recurrent episiotomy in the subsequent delivery (adjusted OR 6.7; 95% CI 6.2–7.3, P < 0.001). The results remained significant for term (adjusted OR 6.8; 95% CI 6.2–7.4, P < 0.001) as well as preterm deliveries (adjusted OR 4.5; 95% CI 3.3–6.3, P < 0.001) in two different models.
Conclusion
Episiotomy is an independent risk factor for recurrent episiotomy in the subsequent delivery.
Similar content being viewed by others
Change history
06 May 2019
The original article can be found online.
References
Harlev A, Pariente G, Kessous R, Aricha-Tamir B, Weintraub AY, Eshkoli T, Dukler D, Ayun SB, Sheiner E (2013) Can we find the perfect oil to protect the perineum? A randomized-controlled double-blind trial. J Matern Fetal Neonatal Med 26(13):1328–1331
Steiner N, Weintraub AY, Wiznitzer A, Sergienko R, Sheiner E (2012) Episiotomy: the final cut? Arch Gynecol Obstet 286(6):1369–1373
Aasheim V, Nilsen ABV, Reinar LM, Lukasse M (2017) Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 6:CD006672. https://doi.org/10.1002/14651858.cd006672.pub3
Carroli G, Mignini L (2009) Episiotomy for vaginal birth. Cochrane Database Syst Rev 1:CD000081. https://doi.org/10.1002/14651858.cd000081.pub2
Homsi R, Daikoku NH, Littlejohn J, Wheeless CR (1994) Episiotomy: risks of dehiscence and rectovaginal fistula. Obstet Gynecol Surv 49:803–808
İsmet G, Bülent D, Özkan Ö (2016) Long and short term complications of episiotomy. Turk J Obstet Gynecol 13:144–148
Sheiner E, Levy A, Walfisch A, Hallak M, Mazor M (2005) Third degree perineal tears in a university medical center, where midline episiotomies are not performed. Arch Gynecol Obstet 271(4):307–310
Labrecque M, Baillargeon L, Dallaire M, Tremblay A, Pinault JJ, Gingras S (1997) Association between median episiotomy and severe perineal lacerations in primiparous women. CMAJ 156:797–802
Fernando R (2007) Risk factors and management of obstetric perineal injury. Obstet Gynecol Reprod Med 17:8
Elliott K (2009) New perinatal quality measures from the National Quality Forum, the Joint Commission and the Leapfrog Group. Curr Opin Obstet Gynecol 21:532–540
Melo et al (2014) Selective episiotomy vs. implementation of a non-episiotomy protocol: a randomized clinical trial. Reprod Health 11:66
Prevention and Management of Obstetric Lacerations at Vaginal (2016) Delivery. Obstetrics and gynecology. Practice bulletin no. 165. American College of Obstetricians and Gynecologists. Obstet Gynecol 128:e1–e15
Antonakou Angeliki, Papoutsis Dimitrios, Henderson Karen, Qadri Zahid, Tapp Andrew (2017) The incidence of and risk factors for a repeat obstetric anal sphincter injury (OASIS) in the vaginal birth subsequent to a first episode of OASIS: a hospital-based cohort study. Arch Gynecol Obstet 295(5):1201–1209
Kleitman V, Feldman R, Walfisch A, Toledano R, Sheiner E (2016) Recurrent shoulder dystocia: is it predictable? Arch Gynecol Obstet 294(6):1161–1166
Corr DT, Hart DA (2013) Biomechanics of scar tissue and uninjured. Skin 2(2):37–43. https://doi.org/10.1089/wound.2011.0321
Corr DT, Gallant-Behm CL, Shrive NG, Hart DA (2009) Biomechanical behavior of scar tissue and uninjured skin in a porcine model. Wound Repair Regen 17:250
White WL, Brody GS, Glaser AA, Marangoni RD, Beckwith TG, Must JS et al (1971) Tensiometric studies of unwounded and wounded skin: results using a standardized testing method. Ann Surg 173:19
Author information
Authors and Affiliations
Contributions
AZ: data collection and manuscript writing. ES: manuscript editing. OB: data analysis. BEH: manuscript editing. TS: project development and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Author A Zilberman declares that she has no conflict of interest. Author E Sheiner declares that he has no conflict of interest. Author O Barret declares that she has no conflict of interest. Author BE Hamou declares that she has no conflict of interest. Author T Silberstein declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
The original version of this article was revised due to a retrospective Open Access Cancellation.
Rights and permissions
About this article
Cite this article
Zilberman, A., Sheiner, E., Barrett, O. et al. Once episiotomy, always episiotomy?. Arch Gynecol Obstet 298, 121–124 (2018). https://doi.org/10.1007/s00404-018-4783-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4783-8