Abstract
Purpose
Ovarian conservation is controversial in patients with cervical adenocarcinoma due to the risk of ovarian metastasis. The aim of this study is to evaluate the association of ovarian conservation with survival outcomes in young patients with T1N0M0 cervical adenocarcinoma.
Methods
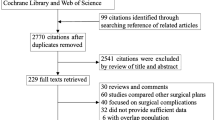
Women who were 45 years of age or younger with T1N0M0 cervical adenocarcinoma from 1988 to 2013 recorded in the Surveillance, Epidemiology, and End Results (SEER) database were included. Propensity score weighting was used to balance the intragroup differences. Cause-specific survival (CSS) and overall survival (OS) were compared using Kaplan–Meier estimates. A multivariate Cox model was used to adjust for covariates including propensity score. A stratified analysis was then conducted.
Results
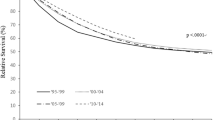
Totally, 1090 (79.7%) patients underwent oophorectomy and 278 (20.3%) patients whose ovaries were preserved were identified. Patients with preserved ovaries were younger, with a lower T classification and less likely to undergo pelvic lymphadenectomy (all p < 0.05). After propensity weighting, ovarian conservation group had better cause-specific survival (CSS) (5-year 98.8 versus 97.1%, 10-year 98.0 versus 95.2%, p = 0.0370) and overall survival (OS) (5-year 98.8 versus 97.1%, 10-year 96.5 versus 93.5%, p = 0.0025). After adjustment, the CSS benefit of ovarian conservation was marginally significant (p = 0.051) and OS benefit was still significant (p = 0.006). Stratified analysis showed that the CSS benefit was found in T1b classification (HR, 0.23; 95% CI 0.06–0.89, p = 0.033) and histological grade > 1 (HR 0.12; 95% CI 0.02–0.87; p = 0.035).
Conclusion
Among young women with T1N0M0 cervical adenocarcinoma, ovarian conservation is associated with better survival.



Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL et al (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108. https://doi.org/10.3322/caac.21262
Koh WJ, Greer BE, Abu-Rustum NR et al (2013) Cervical cancer. J Natl Compr Canc Netw 11:320–343
Plante M (2013) Evolution in fertility-preserving options for early-stage cervical cancer: radical trachelectomy, simple trachelectomy, neoadjuvant chemotherapy. Int J Gynecol Cancer 23:982–989. https://doi.org/10.1097/IGC.0b013e318295906b
Adegoke O, Kulasingam S, Virnig B (2012) Cervical cancer trends in the United States: a 35-year population-based analysis. J Womens Health (Larchmt) 21:1031–1037. https://doi.org/10.1089/jwh.2011.3385
Galic V, Herzog TJ, Lewin SN et al (2012) Prognostic significance of adenocarcinoma histology in women with cervical cancer. Gynecol Oncol 125:287–291. https://doi.org/10.1016/j.ygyno.2012.01.012
Shimada M, Kigawa J, Nishimura R et al (2006) Ovarian metastasis in carcinoma of the uterine cervix. Gynecol Oncol 101:234–237. https://doi.org/10.1016/j.ygyno.2005.10.004
Touhami O, Plante M (2015) Should ovaries be removed or not in (early-stage) adenocarcinoma of the uterine cervix: a review. Gynecol Oncol 136:384–388. https://doi.org/10.1016/j.ygyno.2014.12.011
Takeuchi S (2016) Biology and treatment of cervical adenocarcinoma. Chin J Cancer Res 28:254–262. https://doi.org/10.21147/j.issn.1000-9604.2016.02.11
Sarrel PM, Sullivan SD, Nelson LM (2016) Hormone replacement therapy in young women with surgical primary ovarian insufficiency. Fertil Steril 106:1580–1587. https://doi.org/10.1016/j.fertnstert.2016.09.018
Deb S, Austin PC, Tu JV et al (2016) A review of propensity-score methods and their use in cardiovascular research. Can J Cardiol 32:259–265. https://doi.org/10.1016/j.cjca.2015.05.015
Robins JM, Hernan MA, Brumback B (2000) Marginal structural models and causal inference in epidemiology. Epidemiology 11:550–560
Parker WH, Broder MS, Chang E et al (2009) Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses’ health study. Obstet Gynecol 113:1027–1037. https://doi.org/10.1097/AOG.0b013e3181a11c64
Shuster LT, Rhodes DJ, Gostout BS et al (2010) Premature menopause or early menopause: long-term health consequences. Maturitas 65:161–166. https://doi.org/10.1016/j.maturitas.2009.08.003
Faubion SS, Kuhle CL, Shuster LT et al (2015) Long-term health consequences of premature or early menopause and considerations for management. Climacteric 18:483–491. https://doi.org/10.3109/13697137.2015.1020484
Lokkegaard E, Jovanovic Z, Heitmann BL et al (2006) The association between early menopause and risk of ischaemic heart disease: influence of hormone therapy. Maturitas 53:226–233. https://doi.org/10.1016/j.maturitas.2005.04.009
Macdonald MC, Tidy JA (2016) Can we be less radical with surgery for early cervical cancer? Curr Oncol Rep 18:16. https://doi.org/10.1007/s11912-016-0501-5
Williams NL, Werner TL, Jarboe EA et al (2015) Adenocarcinoma of the cervix: should we treat it differently? Curr Oncol Rep 17:17. https://doi.org/10.1007/s11912-015-0440-6
Kjorstad KE, Bond B (1984) Stage IB adenocarcinoma of the cervix: metastatic potential and patterns of dissemination. Am J Obstet Gynecol 150(3):297–299
Sutton GP, Bundy BN, Delgado G et al (1992) Ovarian metastases in stage IB carcinoma of the cervix: a gynecologic oncology group study. Am J Obstet Gynecol 166:50–53
Natsume N, Aoki Y, Kase H et al (1999) Ovarian metastasis in stage IB and II cervical adenocarcinoma. Gynecol Oncol 74(2):255–258. https://doi.org/10.1006/gyno.1999.5442
Yamamoto R, Okamoto K, Yukiharu T et al (2001) A study of risk factors for ovarian metastases in stage Ib–IIIb cervical carcinoma and analysis of ovarian function after a transposition. Gynecol Oncol 822:312–316. https://doi.org/10.1006/gyno.2001.6277
Kasamatsu T, Onda T, Sawada M et al (2009) Radical hysterectomy for FIGO stage I–IIB adenocarcinoma of the uterine cervix. Br J Cancer 100:1400–1405. https://doi.org/10.1038/sj.bjc.6605048
Ngamcherttakul V, Ruengkhachorn I (2012) Ovarian metastasis and other ovarian neoplasms in women with cervical cancer stage IA–IIA. Asian Pac J Cancer Prev 13(9):4525–4529
Hu T, Wu L, Xing H et al (2013) Development of criteria for ovarian preservation in cervical cancer patients treated with radical surgery with or without neoadjuvant chemotherapy: a multicenter retrospective study and meta-analysis. Ann Surg Oncol 20(3):881–890. https://doi.org/10.1245/s10434-012-2632-8
Kato T, Watari H, Takeda M et al (2013) Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy. J Gynecol Oncol 24(3):222–228. https://doi.org/10.3802/jgo.2013.24.3.222
Chen J, Wang R, Zhang B et al (2016) Safety of ovarian preservation in women with stage I and II cervical adenocarcinoma: a retrospective study and meta-analysis. Am J Obstet Gynecol 215(4):460.e1–460.e13. https://doi.org/10.1016/j.ajog.2016.04.023
Lu H, Li J, Wang L et al (2016) Is ovarian preservation feasible in early-stage adenocarcinoma of the cervix? Med Sci Monit 22:408–414
Zhou J, Chen Y, Zhang P et al (2017) Ovarian preservation in adenocarcinoma of the uterine cervix. J Ovarian Res 10(1):48. https://doi.org/10.1186/s13048-017-0339-y
Jiao XB, Hu J, Zhu LR (2016) The safety of ovarian preservation in early-stage adenocarcinoma compared with squamous cell carcinoma of uterine cervix: a systematic review and meta-analysis of observational studies. Int J Gynecol Cancer 2:1510–1514. https://doi.org/10.1097/IGC.0000000000000780
Hopkins MP, Schmidt RW, Roberts JA, Morley GW (1988) The prognosis and treatment of stage I adenocarcinoma of the cervix. Obstet Gynecol 72:915–921
Matsuo K, Machida H, Shoupe D et al (2017) Ovarian conservation and overall survival in young women with early-stage cervical cancer. Obstet Gynecol 129:139–151. https://doi.org/10.1097/AOG.0000000000001754
Lyu J, Sun T, Tan X (2014) Ovarian preservation in young patients with stage I cervical adenocarcinoma: a surveillance, epidemiology, and end results study. Int J Gynecol Cancer 24:1513–1520. https://doi.org/10.1097/IGC.0000000000000231
Bodner K, Laubichler P, Kimberger O et al (2010) Oestrogen and progesterone receptor expression in patients with adenocarcinoma of the uterine cervix and correlation with various clinicopathological parameters. Anticancer Res 30:1341–1345
Yoo YA, Son J, Mehta FF et al (2013) Progesterone signaling inhibits cervical carcinogenesis in mice. Am J Pathol 183:1679–1687. https://doi.org/10.1016/j.ajpath.2013.07.026
Suzuki Y, Nakano T, Arai T, Morita S, Tsujii H, Oka K (2000) Progesterone receptor is a favorable prognostic factor of radiation therapy for adenocarcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys 47:1229–1234
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
HX: Conception and design, data acquisition, data analysis and interpretation, writing initial draft, writing critical revision, and statistical analysis. XT: Conception and design, data acquisition, data analysis and interpretation, writing initial draft, writing critical revision, and statistical analysis. JD: Conception and design, data acquisition, writing critical revision, statistical analysis. JQ: Conception and design, data analysis and interpretation, writing critical revision. XZ: Conception and design, data analysis and interpretation, writing critical revision. KH: Conception and design, writing critical revision, and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interest to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
The brief abstract was accepted in the meeting of “ESGE 26th Annual Congress”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xu, HY., Tang, X., Ding, J. et al. Ovarian conservation is associated with better survival in young patients with T1N0M0 cervical adenocarcinoma: a population-based study. Arch Gynecol Obstet 297, 775–784 (2018). https://doi.org/10.1007/s00404-018-4674-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4674-z