Abstract
Background
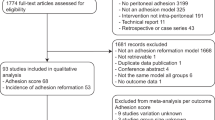
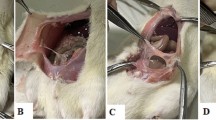
This prospective, randomized, controlled, single-blinded study investigates the peritoneal adhesion formation of HybridAPC (waterjet elevation of the peritoneum with subsequent argon plasma coagulation) versus only waterjet (elevation with the same instrument, but without subsequent argon plasma coagulation) in a rat model (24 female Wistar rats).
Materials and methods
Bilateral lesions were created on the abdominal wall with HybridAPC on one sidewall and waterjet elevation on the other sidewall of the peritoneum in a standard fashion. After 10 days, the rats were euthanized to evaluate the peritoneal trauma sites.
Main outcome measure(s)
Adhesion incidence, quantity, and quality were scored 10 days postoperatively and studied histopathologically.
Result(s)
Incidence of adhesion formation was 2.3% for HybridAPC; no adhesions occurred for peritoneal elevation with saline (p = 1.00). Histologic evaluation revealed no acute inflammation in both groups. An overall moderate degree of granulation tissue formation and myonecrosis was observed in the HybridAPC group, whereas no chronic inflammation and myonecrosis occurred after elevation without thermal ablation (p < 0.0001).
Conclusion(s)
This study investigates the effect of waterjet elevation of the peritoneum with and without subsequent thermal ablation on adhesion formation in a rat model for the first time. Peritoneal waterjet elevation with saline does not provide any risk of adhesion formation. Thermal coagulation with APC after waterjet elevation of the peritoneum creates advantageous peritoneal conditions due to a permanent moist tissue surface and the cooling effect of the injected solution, resulting in no significant difference in adhesion formation compared to peritoneal elevation without thermal ablation. HybridAPC can thus be regarded as a beneficial coagulation method with only minor adhesion formation due to positive tissue effects of the combined waterjet.




Similar content being viewed by others
References
Rajab TK, Wallwiener M, Talukdar S et al (2009) Adhesion-related complications are common, but rarely discussed in preoperative consent: a multicenter study. World J Surg 33(4):748–750. https://doi.org/10.1007/s00268-008-9917-x
Boland GM, Weigel RJ (2006) Formation and prevention of postoperative abdominal adhesions. J Surg Res 132(1):3–12. https://doi.org/10.1016/j.jss.2005.12.002
Wallwiener CW, Kraemer B, Wallwiener M et al (2010) The extent of adhesion induction through electrocoagulation and suturing in an experimental rat study. Fertil Steril 93(4):1040–1044. https://doi.org/10.1016/j.fertnstert.2008.12.002
Kraemer B, Rothmund R, Fischer K et al (2011) A prospective, randomized, experimental study to investigate the peritoneal adhesion formation of noncontact argon plasma coagulation in a rat model. Fertil Steril 95(4):1328–1332. https://doi.org/10.1016/j.fertnstert.2011.01.138
Kraemer B, Scharpf M, Planck C et al (2014) Randomized experimental study to investigate the peritoneal adhesion formation of conventional monopolar contact coagulation versus noncontact argon plasma coagulation in a rat model. Fertil Steril 102(4):1197–1202. https://doi.org/10.1016/j.fertnstert.2014.07.007
Vetere PF, Lazarou G, Apostol R et al (2015) Postoperative adhesion formation in a rabbit model: monopolar electrosurgery versus ultrasonic scalpel. JSLS 19(2):e2015. https://doi.org/10.4293/jsls.2015.00018
Kraemer B, Rothmund R, Fischer K et al (2014) A prospective experimental study to investigate the peritoneal adhesion formation of argon plasma coagulation (APC) versus a novel aerosol plasma in a rat model. Surg Innov 21(4):389–397. https://doi.org/10.1177/1553350613506300
Kashin SV, Kuvaev R, Nadezhin AS et al (2016) Mo2016 the new hybrid argon plasma coagulation (HybridAPC) for endoscopic ablation of Barrett’s esophagus (BE): the results of the pilot trial. Gastrointest Endosc 83(5):AB495. https://doi.org/10.1016/j.gie.2016.03.708
Manner H, Neugebauer A, Scharpf M et al (2014) The tissue effect of argon-plasma coagulation with prior submucosal injection (Hybrid-APC) versus standard APC: a randomized ex vivo study. United Eur Gastroenterol J 2(5):383–390. https://doi.org/10.1177/2050640614544315
Sharjeel Arshad HM, Ahsan N, Aldridge T et al (2017) Tu1161 safety and efficacy of endoscopic HybridAPC for management of Barrett’s esophagus. Gastrointest Endosc 85(5):AB562–AB563. https://doi.org/10.1016/j.gie.2017.03.1298
Manner H, May A, Kouti I et al (2016) Efficacy and safety of Hybrid-APC for the ablation of Barrett’s esophagus. Surg Endosc 30(4):1364–1370. https://doi.org/10.1007/s00464-015-4336-1
Rösch T, Manner H, May A et al (2017) 1151 multicenter feasibility study of combined injection and argon plasma coagulation (Hybrid-APC) in the ablation therapy of neoplastic Barrett esophagus. Gastrointest Endosc 85(5):AB154. https://doi.org/10.1016/j.gie.2017.03.331
Wallwiener M, Brucker S, Hierlemann H et al (2006) Innovative barriers for peritoneal adhesion prevention: liquid or solid? A rat uterine horn model. Fertil Steril 86(4 Suppl):1266–1276. https://doi.org/10.1016/j.fertnstert.2006.05.023
Han ES, Scheib SA, Patzkowsky KE et al (2017) The sticky business of adhesion prevention in minimally invasive gynecologic surgery. Curr Opin Obstet Gynecol 29(4):266–275. https://doi.org/10.1097/gco.0000000000000372
Cwalinski J, Staniszewski R, Baum E et al (2015) Normal saline may promote formation of peritoneal adhesions. Int J Clin Exp Med 8(6):8828–8834
Polubinska A, Breborowicz A, Staniszewski R et al (2008) Normal saline induces oxidative stress in peritoneal mesothelial cells. J Pediatr Surg 43(10):1821–1826. https://doi.org/10.1016/j.jpedsurg.2008.02.010
Lindor LJ, Loegering DA, Wassom DL et al (1981) Recovery of eosinophils from the peritoneal cavity of the guinea pig. J Immunol Methods 41(1):125–134
Hellman C, Lundahl J, Hylander B et al (2000) Phenotypic alterations of recruited eosinophils in peritoneal fluid eosinophilia. Perit Dial Int 20(3):295–300
Edelstam G, Fredens K, Venge P (1994) Role of eosinophilic granulocytes in women with infertility and pelvic adhesions. Inflammation 18(4):361–371
Ott DE (2008) Laparoscopy and adhesion formation, adhesions and laparoscopy. Semin Reprod Med 26(4):322–330. https://doi.org/10.1055/s-0028-1082390
Gomel V, Koninckx PR (2016) Microsurgical principles and postoperative adhesions: lessons from the past. Fertil Steril 106(5):1025–1031. https://doi.org/10.1016/j.fertnstert.2016.08.040
Breborowicz A, Oreopoulos DG (2005) Is normal saline harmful to the peritoneum? Perit Dial Int 25(Suppl 4):S67–S70
Tarhan OR, Barut I, Sezik M (2008) An evaluation of normal saline and taurolidine on intra-abdominal adhesion formation and peritoneal fibrinolysis. J Surg Res 144(1):151–157. https://doi.org/10.1016/j.jss.2007.09.006
Rajab TK, Smaxwil L, Wallwiener M (2013) Animal model for local pharmacotherapy in adhesion prophylaxis—a proof of concept. J Investig Surg 26(4):200–203. https://doi.org/10.3109/08941939.2012.741657
Rajab TK, Kraemer B, Petri N et al (2012) Intra-operative locally injected pharmacotherapy as a novel strategy for adhesion prophylaxis. Int J Surg 10(9):489–492. https://doi.org/10.1016/j.ijsu.2012.07.003
Norton ID, Wang L, Levine SA et al (2002) In vivo characterization of colonic thermal injury caused by argon plasma coagulation. Gastrointest Endosc 55(6):631–636
Al-Alem I, Pillai K, Akhter J et al (2014) Heat sink phenomenon of bipolar and monopolar radiofrequency ablation observed using polypropylene tubes for vessel simulation. Surg Innov 21(3):269–276. https://doi.org/10.1177/1553350613505713
Zorbas G, Samaras T (2015) A study of the sink effect by blood vessels in radiofrequency ablation. Comput Biol Med 57:182–186. https://doi.org/10.1016/j.compbiomed.2014.12.014
Author information
Authors and Affiliations
Contributions
BK: protocol/project development, data analysis, manuscript writing, and editing. MS: data collection, data analysis, and manuscript writing. SK: protocol/project development and data collection. JD: protocol/project development and data collection. CT: protocol/project development. KB: protocol/project development, data collection, data management, data analysis, and manuscript writing. MDE: protocol/project development and data analysis. AN: protocol/project development and data analysis. DN: data collection, data analysis, and manuscript writing. FF: protocol/project development and data analysis. SB: protocol/project development and data analysis. FAT: data analysis and editing. SK: data collection. RR: protocol/project development and data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors B. Kraemer, M. Scharpf, S. Keckstein, J. Dippon, C. Tsaousidis, F. Fend, S. Brucker, F. A. Taran, S. Kommoss, and R. Rothmund have no conflicts of interest to disclose in relation to the submitted manuscript. The authors K. Brunecker, M. D. Enderle, A. Neugebauer, and D. Nuessle are employees of Erbe research department, Germany.
Ethical approval
All applicable institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Rights and permissions
About this article
Cite this article
Kraemer, B., Scharpf, M., Keckstein, S. et al. A prospective randomized experimental study to investigate the peritoneal adhesion formation after waterjet injection and argon plasma coagulation (HybridAPC) in a rat model. Arch Gynecol Obstet 297, 961–967 (2018). https://doi.org/10.1007/s00404-018-4661-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4661-4