Abstract
Purpose
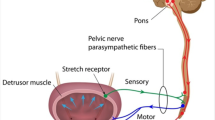
Clinical relevance of neurological evaluation in patients suffered urinary retention in the absence of subvesical obstruction. Determining whether (1) women complaining residual bladder volume without prolapse and obstruction always suffer pudendal nerve damage; (2) neurogenic damage can be linked to patients history/clinical examination; (3) therapy alters regarding to neurological findings; and (4) electromyography (EMG) of musculus sphincter ani externus (MSAE) can be omitted with electronically stimulated pudendal nerve latency (ESPL) as the standard investigation.
Methods
Women with urinary retention without ≥stage 2 prolapse or obstruction have neurological investigation including vaginally and anally pudendal terminal nerve latency (PTNL) (>2.4 ms considered abnormal) and EMG seen 7/2005-04/2010.
Results
(1) 148/180 (82.2%) suffered at least moderate neurogenic damage and (2) severe neurogenic damage occurs with urge odds ratio (OR) = 3.1 or age (OR = 3.2). Correlations: spasticity with therapy changes (OR = 11.1), latencies. (a) Anally: (i) right and peripheral neuropathy (PNP) (OR = 2.5), chemotherapy (OR = 5.0); (ii) left and PNP (OR = 3.9), chemotherapy (OR = 4.8); (iii) left or right with PNP (OR = 3.9), chemotherapy (OR = 6.8); and (iv) left and right with chemotherapy (OR = 5.0). (b) Vaginally: (i) right with age >60 (OR = 3.2), radical operation (OR = 10.6); (ii) left with diabetes mellitus (OR = 2.5); and (iii) left or right with age (OR = 3.3), radical operation (OR = 8.7). (3) 19.6% therapy changes (36 patients). (4) Neither EMG nor ESPL can be replaced one by another (p = 0.12 anal, p = 0.05 vaginal).
Conclusion
Red flags are neurogenic damage, age >60, chemotherapy, PNP, radical operation or diabetes. In unclear situations, EMG and ESPL need to be performed to gain relevant information.

Similar content being viewed by others
References
Jeon S, Yoo EH (2012) Predictive value of obstructive voiding symptoms and objective bladder emptying tests for urinary retention. J Obstet Gynaecol 32(8):770–772
Sangwan YP, Coller JA, Barrett MS, Murray JJ, Roberts PL, Schoetz DJ Jr (1996) Unilateral pudendal neuropathy. Significance and implication. Dis Colon Rectum 39(3):249–251
Jameson JS, Rogers J, Chia YW, Misiewicz JJ, Henry MM, Swash M (1994) Pelvic floor function in multiple sclerosis. Gut 35(3):388–390
Sørensen M, Lorentzen M, Petersen J, Christiansen J (1991) Anorectal dysfunction in patients with urologic disturbance due to multiple sclerosis. Dis Colon Rectum 34(2):136–139
Fowler AL, Mills A, Durdey P, Thomas MG (2005) Single-fiber electromyography correlates more closely with incontinence scores than pudendal nerve terminal motor latency. Dis Colon Rectum 48(12):2309–2312
Kavia RB, Datta SN, Dasgupta R, Elneil S, Fowler CJ (2006) Urinary retention in women: its causes and management. BJU Int. 97(2):281–287
Sylvester PA, McLoughlin J, Sibley GN, Dorman PJ, Kabala J, Ormerod IE (1995) Neuropathic urinary retention in the absence of neurological signs. Postgrad Med J 71(842):747–748
Jost W (2008) Stellenwert neurophysiologischer Untersuchungen bei Funktionsstörungen des Beckenbodens. Das Neurophysiologie Labor 30:140–152
Cavalcanti GA, Manzano GM, Giuliano LM, Nobrega JA, Srougi M, Bruschini H (2006) Pudendal nerve latency time in normal women via intravaginal stimulation. Int Braz J Urol. 32(6):705–711 (discussion 712)
Wiesner A, Jost W (2001) Vaginal versus anal stimulierte Pudenduslatenz- ein Vergleich. Akt Neurol 28:388–390
Tetzschner T, Sørensen M, Lose G, Christiansen J (1997) Vaginal pudendal nerve stimulation: a new technique for assessment of pudendal nerve terminal motor latency. Acta Obstet Gynecol Scand 76(4):294–299
Kim SJ, Kim WR, Kim HS, Park HW, Cho YW, Jang SH, Hwang SJ, Ahn SH (2011) Abnormal spontaneous activities on needle electromyography and their relation with pain behavior and nerve fiber pathology in a rat model of lumbar disc herniation. Spine (Phila Pa 1976) 36(24):E1562–E1567
Ross JW (2001) Laparoscopic Burch colposuspension and overlapping sphincteroplasty for double incontinence. JSLS. 5(3):203–209
Lombardi G, Musco S, Celso M, Del Corso F, Del Popolo G (2014) Sacral neuromodulation for neurogenic non-obstructive urinary retention in incomplete spinal cord patients: a ten-year follow-up single-centre experience. Spinal Cord. 52(3):241–245
Sanford MT, Suskind AM (2016) Neuromodulation in neurogenic bladder. Transl Androl Urol 5(1):117–126
Azaïs H, Rubod C, Ghoneim T, Vassilieff M, Bailly E, Boileau L, Villet R, Collinet P (2015) Persistent urinary retention after surgery for deep infiltrating endometriosis: a multi-center series of 16 cases. Arch Gynecol Obstet 291(6):1333–1339
Fanfani F, Costantini B, Mascilini F, Vizzielli G, Gallotta V, Vigliotta M, Piccione E, Scambia G, Fagotti A (2015) Early postoperative bladder training in patients submitted to radical hysterectomy: is it still necessary? A randomized trial. Arch Gynecol Obstet 291(4):883–888
Snooks SJ, Henry MM, Swash M (1985) Faecal incontinence due to external anal sphincter division in childbirth is associated with damage to the innervation of the pelvic floor musculature: a double pathology. Br J Obstet Gynaecol 92(8):824–828
Snooks SJ, Henry MM, Swash M (1985) Anorectal incontinence and rectal prolapse: differential assessment of the innervation to puborectalis and external anal sphincter muscles. Gut 26(5):470–476
Wietek BM, Hinninghofen H, Jehle EC, Enck P, Franz HB (2007) Asymmetric sphincter innervation is associated with fecal incontinence after anal sphincter trauma during childbirth. Neurourol Urodyn 26(1):134–139
Baig MK, Wexner SD (2000) Factors predictive of outcome after surgery for faecal incontinence. Br J Surg 87(10):1316–1330
Gilliland R, Altomare DF, Moreira H Jr, Oliveira L, Gilliland JE, Wexner SD (1998) Pudendal neuropathy is predictive of failure following anterior overlapping sphincteroplasty. Dis Colon Rectum. 41(12):1516–1522
Lacima G, Pera M, Valls-Solé J, González-Argenté X, Puig-Clota M, Espuña M (2006) Electrophysiologic studies and clinical findings in females with combined fecal and urinary incontinence: a prospective study. Dis Colon Rectum 49(3):353–359
Smith AR, Hosker GL, Warrell DW (1989) The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine. A neurophysiological study. Br J Obstet Gynaecol 96(1):24–28
Snooks SJ, Setchell M, Swash M, Henry MM (1984) Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet 2(8402):546–550
Snooks SJ, Swash M, Henry MM, Setchell M (1986) Risk factors in childbirth causing damage to the pelvic floor innervation. Int J Colorectal Dis 1(1):20–24
Snooks SJ, Swash M, Mathers SE, Henry MM (1990) Effect of vaginal delivery on the pelvic floor: a 5-year follow-up. Br J Surg. 77(12):1358–1360
Allen RE, Hosker GL, Smith AR, Warrell DW (1990) Pelvic floor damage and childbirth: a neurophysiological study. Br J Obstet Gynaecol 97(9):770–779
South MM, Stinnett SS, Sanders DB, Weidner AC (2009) Levator ani denervation and reinnervation 6 months after childbirth. Am J Obstet Gynecol 200(5):519.e1
Weidner AC, Jamison MG, Branham V, South MM, Borawski KM, Romero AA (2006) Neuropathic injury to the levator ani occurs in 1 in 4 primiparous women. Am J Obstet Gynecol. 195(6):1851–1856
Pifarotti P, Gargasole C, Folcini C, Gattei U, Nieddu E, Sofi G, Buonaguidi A, Meschia M (2014) Acute post-partum urinary retention: analysis of risk factors, a case-control study. Arch Gynecol Obstet. 289(6):1249–1253
Henry MM, Parks AG, Swash M (1980) The anal reflex in idiopathic faecal incontinence: an electrophysiological study. Br J Surg 67(11):781–783
Author information
Authors and Affiliations
Contributions
Each authors´ contribution to the work: NS-T—data collection and manuscript writing; AH-W—examiner and editing manuscript; CE—research fellow and data collection; KB—editing manuscript; FS—statistics; and RT—manuscript idea and editing manuscript.
Corresponding author
Ethics declarations
Funding
This study was not funded.
Conflict of interest
Author Schwertner-Tiepelmann declares the following: receiving travel expenses and fee for participation at expert meetings (Medtronic) 2016/2017 as well as conducting an ultrasound study sponsored by Lilly 2010/2011. The other authors do not have anything to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was conducted by the local committee (Charité’s Ethics Committee) EA1/218/15. Informed consent was obtained from all individuals participants included in the study.
Rights and permissions
About this article
Cite this article
Schwertner-Tiepelmann, N., Hagedorn-Wiesner, A., Erschig, C. et al. Clinical relevance of neurological evaluation in patients suffering urinary retention in the absence of subvesical obstruction. Arch Gynecol Obstet 296, 1017–1025 (2017). https://doi.org/10.1007/s00404-017-4519-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4519-1